PGT Testing IVF Cost: Complete 2026 Pricing Guide
Your clinic quoted $4,500 for PGT. But the frozen transfer is another $5,000. Your medications jumped $2,000. Suddenly your $15K IVF cycle is $26,500.
Preimplantation genetic testing (PGT) pricing is deliberately confusing. Hidden fees, per-embryo charges, and bundled costs vary 300% between clinics. One charges $2,500. Another charges $8,000. Same test. Same genetics labs, often.
In this pricing guide, you’ll learn:
- Exact cost breakdowns for every fee.
- Per-embryo math showing what you’ll actually pay.
- Insurance coverage exceptions (including California’s SB 729).
- Cost-reduction strategies that save 20-30%.
Here’s every cost, exposed. No jargon. No surprise bills.
How Much Does PGT Testing Cost in 2026
National Average PGT-A Costs by Clinic Type
PGT-A testing (preimplantation genetic screening for chromosomal abnormalities) ranges from $2,000 to $10,000 nationally, with most clinics charging $4,000-$6,000.
Why the 400% variance? Location (NYC vs. Syracuse = $4,000 difference), clinic volume (high-volume clinics negotiate better rates), and billing structure (bundled vs. itemized) significantly impact your bill.
| Clinic Type | PGT-A Base | Per Embryo Fee | Total for 5 Embryos |
|---|---|---|---|
| Budget | $2,000-$3,000 | $0-$300 each | $2,000-$4,500 |
| Mid-tier | $4,000-$6,000 | Usually included | $4,000-$6,000 |
| High-end | $7,000-$10,000 | Usually included | $7,000-$10,000 |
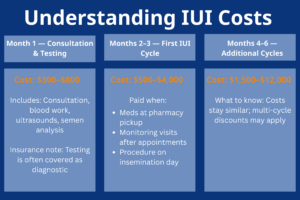
The FET Trap: Why Your PGT Cost is Always Higher Than Quoted
Every PGT cycle requires a frozen embryo transfer. PGT results take 7-14 days. Your embryos get biopsied, then frozen while the lab analyzes them. Fresh transfer becomes impossible.
What FET actually costs:
- Budget clinics: $1,900-$2,500.
- Mid-tier clinics: $3,500-$5,000.
- High-end clinics: $5,000-$7,000.
The real math: Clinic quotes $5,000 for PGT, but they don’t always mention the $4,500 FET. Your actual cost: $9,500.
What you’re paying for: 3-4 lining check ultrasounds, estrogen/progesterone medications, transfer procedure, pregnancy test.
Per-Embryo Pricing Models: How Your Embryo Count Drives Costs
Not all clinics charge the same way. Some charge flat rates. Others add fees beyond a certain embryo count.
| Embryo Count | Flat-Rate Clinic | Per-Embryo Clinic (base + $350 over 5) |
|---|---|---|
| 3 embryos | $4,500 | $4,500 |
| 5 embryos | $4,500 | $4,500 |
| 8 embryos | $4,500 | $5,550 |
| 10 embryos | $4,500 | $6,250 |
| 15 embryos | $4,500 | $7,900 |
The cruel irony: “Great news, you have 10 viable embryos!” also means “$2,500 more in testing fees you didn’t budget for.”
This hits egg donor cycles hardest. Donor cycles often yield 15-20 embryos. If your clinic charges per embryo, that’s $4,000-$6,000 in extra fees.
Biopsy Fees vs. Lab Fees: Understanding the Two-Part Bill
Your preimplantation genetic testing bill has two parts. Many clinics don’t explain this upfront.
Part 1: Clinic embryo biopsy fees ($1,500-$3,000)
What you’re paying for: Embryologist time, specialized equipment, cell extraction at blastocyst stage, embryo freezing post-biopsy.
Part 2: Genetics lab fees ($2,500-$7,000)
What you’re paying for: Chromosome analysis, genetic counseling, results report, data storage. This is performed in labs, such as Natera, Igenomix, CooperGenomics.
How you get billed:
- Bundled: One price, one charge.
- Itemized: Clinic charges biopsy upfront, genetics lab bills you separately 2-4 weeks later (surprise bill).
If your clinic only quotes the biopsy fee ($1,800), expect a $3,500 lab bill later.

PGT-M and PGT-SR: Why Single-Gene Testing Costs $3K-$5K More
If you need testing for specific genetic disorders or structural rearrangements, costs jump 50-100%.
Cost comparison:
- PGT-A (aneuploidy): $4,000-$7,000.
- PGT-M (single gene disorders): $7,000-$12,000.
- PGT-SR (structural rearrangements): $7,000-$10,000.
Why PGT-M costs more:
- Custom probe development for your specific genetic disease ($900-$1,900).
- Family blood testing ($300-$500).
- Mandatory genetic counseling sessions ($500-$1,200).
- Lower patient volume = higher per-case costs.
Real cost breakdown (PGT-M for cystic fibrosis):
| Line Item | Cost |
|---|---|
| Probe setup | $1,200 |
| Clinical testing | $2,600 |
| Embryo biopsy | $1,800 |
| Genetic counseling | $800 |
| FET cycle | $4,000 |
| Total | $10,400 |
Regional Cost Differences: What LA Patients Need to Know
Geographic location drives major price variance:
- Rural/small cities: $2,500-$4,000.
- Mid-size metros: $4,000-$5,500.
- Major metros (LA, NYC, SF): $6,000-$9,000.
- Ultra-premium markets: $8,000-$10,000.
Los Angeles falls into the major metro category at $6,000-$9,000 for PGT-A. This isn’t price gouging: overhead in LA is genuinely 2-3x higher.
At California Center for Reproductive Health, we’ve built our practice around value-focused pricing that rivals mid-tier markets, without compromising on success rates.
Plus, the California SB 729 fertility coverage mandate may cover significant portions of your IVF and preimplantation genetic testing costs if you have qualifying insurance; something unavailable if you travel out of state (more on this below).

Insurance Coverage for PGT Testing: What’s Covered and What’s Not
The Hard Truth About PGT Insurance Coverage
95% of insurance plans exclude preimplantation genetic testing, even when they fully cover IVF cycles. Your insurance approves $20,000 for IVF (medications, monitoring, egg retrieval, embryo culture, fresh transfer). Then you ask about preimplantation genetic testing. Denied.
You’re out-of-pocket for the entire $5,000-$7,000 PGT cost PLUS the $4,000-$6,000 frozen embryo transfer.
Why insurers exclude it: PGT is classified as “experimental” (despite 20+ years of use) and considered “not medically necessary” for routine IVF patients. Adding PGT-A to every IVF cycle would increase insurance payouts 30-40%.
When coverage might happen (rare exceptions):
- Known genetic disease carriers (PGT-M): 30-40% approval rate if you’re a documented carrier for cystic fibrosis, sickle cell, Tay-Sachs, BRCA, or Huntington’s. Insurers prefer paying $8,000 for testing vs. $500K-$2M lifetime costs for an affected child. Required for approval: genetic testing results, genetic counseling notes (2+ sessions), fertility specialist letter.
- Recurrent pregnancy loss: 10-20% approval rate with 2-3+ documented miscarriages showing chromosomal abnormalities. Required for approval: miscarriage records, karyotype testing of pregnancy loss tissue, fertility specialist letter, genetic counseling notes. You also get better odds if you’re 35+ with 3+ losses.
- Structural chromosomal rearrangement (PGT-SR): 25-35% approval rate if one partner has balanced translocation or inversion (50-80% risk of aneuploid embryos). Required for approval: karyotype results, genetic counseling, physician letter.
- Advanced maternal age + failed IVF: 5-10% approval rate (very rare) if you’re 38+ with 1-2+ failed transfers. Required for approval: prior cycle records, AMH/FSH results, specialist letter. Most insurers deny it, but Blue Cross and Cigna occasionally approve it.
California’s SB 729: Game-Changer for IVF and PGT Coverage
If you live in California with insurance through an employer with 51+ employees, SB 729 may cover your preimplantation genetic testing. This is new (started on January 1st, 2026) and many patients don’t know about it yet.
What SB 729 covers:
- Mandates coverage for “fertility services including IVF, embryo transfer, and related laboratory procedures”.
- Up to 3 egg retrievals OR $30,000 in fertility benefits (whichever comes first).
- No lifetime limit on embryo transfers.
- “Related laboratory procedures” may include PGT-A testing and PGT-M (depends on your plan’s interpretation).
Who qualifies:
- California residents with insurance from employers with 51+ employees.
- Applies to fully-insured plans (most common).
- Does NOT apply to self-funded employer plans (about 30% of large employers), Medicare, or Medi-Cal.
What this means for your costs:
If SB 729 covers PGT: Your $5,000 PGT-A cost and $4,500 FET may be fully covered, saving you $9,500 out-of-pocket.
If SB 729 covers IVF but excludes PGT: You’ll still save $15,000-$20,000 on the IVF cycle, but pay out-of-pocket for PGT and FET.
Action steps:
- Call your insurance and ask: “Does my plan comply with California SB 729 fertility coverage mandate?”
- Then ask: “Does the coverage include preimplantation genetic testing PGT-A and PGT-M?”
- Request written confirmation; phone reps make mistakes.
At California Center for Reproductive Health, we help you navigate SB 729 coverage, submit pre-authorizations, and maximize your benefits. We’ve helped hundreds of patients access their new California fertility benefits.

Strategic Cost-Reduction Tactics
Partial Testing: Test Your Top-Graded Embryos Only
Instead of testing all your embryos upfront, test only the 3-4 highest-graded ones first. If those result in a successful pregnancy, you never need to pay to test the rest.
The math works out like this: If you have 10 embryos and your fertility clinic charges $400 per embryo over 5, testing all 10 costs $6,100 total. Testing only your top 4 embryos costs just the $4,500 base price. That’s $1,600 in savings.
How the strategy works: Your embryos get graded AA, AB, BA, BB based on quality at blastocyst stage. AA and AB grade embryos have the best morphology with 60-70% euploid rates. Lower grades drop to 30-40% euploid rates. Test your best embryos first. If one tests normal and leads to pregnancy, you’re done. If they test abnormal or fail implantation, you can test the remaining embryos later.
The tradeoff: You might pay embryo biopsy fees twice if you need a second round. But if your top embryos work, you save money and avoid unnecessary testing of embryo cells.
This is the best option for many patients with 8+ embryos on tight budgets. Skip this if you only have 3-5 embryos total or you’re over 40 (even best embryos often have genetic abnormality issues at that age).
Use HSA/FSA Accounts to Save 20-30% on Taxes
Preimplantation genetic diagnosis and preimplantation genetic screening are both HSA/FSA eligible. You save 20-30% automatically by using pre-tax dollars for your fertility treatment.
How the tax savings work: You contribute pre-tax dollars to your HSA or FSA, saving your marginal tax rate plus FICA (7.65%). If you’re in the 24% tax bracket, you save 31.65% total. So $8,000 in PGT results and FET costs effectively becomes $5,468 after tax savings. That’s $2,532 back in your pocket.
FSA (Flexible Spending Account): 2026 limit is $3,300. Funds are available immediately on January 1. The catch is use-it-or-lose-it by year end, though some plans offer a 2.5 month grace period.
Example: $5,000 PGT-A cost. Use $3,300 from FSA (saves $1,045 in taxes). Pay $1,700 out-of-pocket. Your effective cost is $3,955.
HSA (Health Savings Account): 2026 limits are $4,300 individual / $8,550 family. Funds roll over year to year with no expiration. You need a high-deductible health plan to qualify. Many IVF patients build HSA balances over 2-3 years before starting treatment.
Example: Save $8,000 in HSA over two years. Use for PGT ($5,000) and FET ($4,500). Tax savings at 31.65% rate: $2,530.
What’s covered: Embryo biopsy fees, genetics lab fees, genetic counseling, embryo freezing, FET cycle, FET medications.
Smart timing: If your IVF treatment spans two calendar years, max out FSA both years. Do egg retrieval December 2025, then PGT and FET January 2026. Use 2025 FSA ($3,200) for IVF, 2026 FSA ($3,300) for PGT. Total savings: $2,058.
Explore Financing Options and Grants
Fertility financing companies like Sunfish and Kindbody specialize in fertility loans with payment plans. You apply online, get approved in 24-48 hours, they pay your fertility clinic directly, then you make monthly payments.
Example: Borrow $10,000 at 7% APR over 5 years = $198/month payment.
Credit cards with 0% intro APR work for short-term financing. Cards like Chase Sapphire, Citi Diamond Preferred, BankAmericard offer 12-18 months interest-free. Put your $9,500 PGT plus FET cost on the card, pay $528/month for 18 months to clear before interest hits. Just make sure you pay it off before the promo ends or you’ll face 20%+ rates.
Grants provide free money for fertility treatment, though they’re competitive.
- Baby Quest Foundation awards up to $15,000 (apply February and October).
- Cade Foundation offers $5,000-$10,000 for military families and first responders.
- Pay It Forward Fertility provides $2,000-$5,000.
- Tinina Q. Cade Foundation awards $5,000-$8,000 for women of color.
Reality check: Thousands apply for limited spots. You need essays about your fertility journey, financial hardship docs, and physician letters. Start applications 6+ months early and apply to multiple grants simultaneously to maximize your chances.
Employer benefits are increasingly common. Check if your company covers PGT-A costs as part of fertility benefits. If your employer uses Carrot, Progyny, or Maven, genetic testing is usually covered.
Stop Guessing About PGT Costs: Get Your Personalized Quote
PGT pricing varies wildly ($2,000-$10,000), comes with often hidden FET costs, and per-embryo fees catch patients off-guard.
Transparency matters. At California Center for Reproductive Health, we provide upfront, itemized pricing with no surprise bills. Our fertility specialists work with IVF patients to create clear paths to successful pregnancy. Plus our team helps you navigate SB 729 benefits to maximize coverage for PGT and IVF treatment.
Ready for your exact cost? Schedule a free consultation at our fertility clinic for a personalized breakdown based on your age, expected embryo count, and insurance coverage.