Mini IVF in Los Angeles
Minimal in vitro fertilization (mini IVF) is a unique IVF protocol in which low-dose hormone stimulation is used to achieve excellent pregnancy rates without many of the side effects of traditional IVF. Many patients in the Los Angeles area have come to Dr. Mor for his expertise with the minimal IVF treatment.
Mini IVF
Mini IVF, also known as “minimal stimulation IVF,” or “Micro IVF,” is a relatively new and advanced reproductive technology (ART) that offers a gentle alternative of ovarian stimulation to traditional in vitro fertilization (IVF). In Mini IVF the ovaries of a woman are minimally stimulated, using oral ovulation induction agents (Clomid, Tamoxifen, Letrozole…) and/or low doses of gonadotropins (follicle stimulating hormone and luteinizing hormone), in order to induce the growth of a small cohort of eggs. Once mature, the eggs are retrieved in a minor surgical procedure and fertilized in the IVF lab; the resulting embryos are transferred back into the woman’s uterus. The process is identical to traditional IVF, except that the goal is to create only a few but high-quality embryos for transfer. Mini IVF answers two major concerns for both patient and doctor — cost and overmedication. Recent trends in the fertility field prefer an ovulation induction that uses fewer medications and produces fewer but better quality embryos than an ovulation induction that uses significantly higher doses of medications. In other words, Mini-IVF is a useful method that can be used to help women get pregnant with minimal risks and low cost.
Mini IVF is an excellent ART tool which bridges the gap between Natural Cycle IVF and traditional IVF. While in Natural cycle IVF no ovarian stimulation is performed (no oral and/or injectable medications are taken), typically yielding only 1-2 naturally grown eggs and one embryo, in Mini IVF a “gentle” ovarian stimulation yields 3-4 eggs and 2-3 embryos, increasing the cycle efficiency significantly. Whereas in traditional IVF a high dose of gonadotropins is often used to maximize eggs/embryos from a single cycle, in Mini-IVF it is egg and embryo quality which is maximized rather than the number.
Couples who choose the Mini IVF treatment hope to obtain more eggs than in Natural Cycle IVF while avoiding some of the discomforts, risks, and costs which may be associated with traditional IVF. As such, patients undergoing Mini IVF may achieve the following benefits:
-
- Minimize exposure to drugs during ovarian stimulation and at the time of egg retrieval,
- Reduce health risks and discomfort caused by ovarian hyperstimulation syndrome (OHSS),
- Eliminate or significantly reduce the pain of daily drug injections,
- Reduce the high cost of drugs, and
- Shorter wait time between cycles.
How is Mini IVF done?
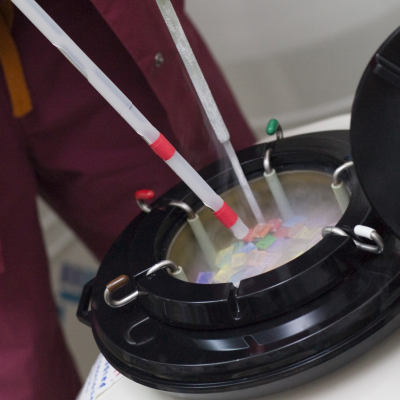
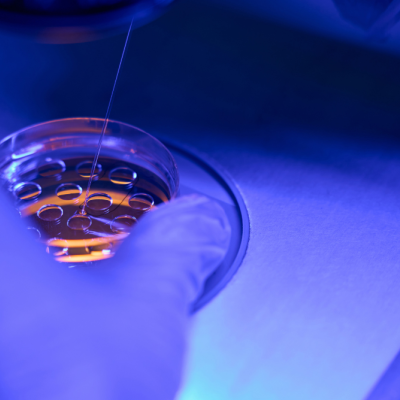
Mini IVF protocols may differ slightly from clinic to clinic but share a common goal: a gentle mild stimulation of the ovaries for the purpose of obtaining a small number of high-quality eggs and embryos. Most Mini IVF protocols begin with a short course of birth control pills (oral contraceptive pills=OCPs) followed by ovarian stimulation with oral ovulation induction agents (Clomid, Tamoxifen, Letrozole…). In patients older than 35 years of age, some protocols will forgo the use of OCPs and begin stimulation of the ovaries on day 2-3 of the menstrual cycle. Many Mini IVF protocols will involve the addition of low doses of injectable gonadotropins to orally ingested ovulation induction agents (often referred to as Micro IVF), while other protocols rely on low doses of gonadotropins only for ovarian stimulation. Monitoring is primarily by ultrasound exams with a minimal number of blood tests. The egg retrieval procedure is identical to that done in traditional IVF, except that some patients will prefer to avoid intravenous sedation (anesthesia) since only a small number of eggs are harvested, and choose to undergo the procedure with oral analgesia (pain medications) only. Eggs are fertilized in the IVF lab with either standard insemination (mixing of sperm with eggs) when no male factor exists or with intracytoplasmic sperm injection (ICSI) in cases where male factor infertility exists. Embryos may be transferred back into the uterus when they are 3, 4, 5 or 6 days old.
The main objectives are to create 2-3 good quality embryos and to make the procedure as simple as possible for the patient. The entire process takes place over about 7-10 days. The trade-off of possibly having to do more cycles to achieve pregnancy is compensated for by a lower cost and an easier experience.
How much does Mini IVF cost?
The total cost for Mini IVF is typically more than half that of a traditional IVF cycle. Costs include medications, office monitoring visits, anesthesia costs, and IVF specific procedure and laboratory costs. Some patients will have some of these costs covered by their insurance.
Who should consider Mini-IVF?
The choice of Mini IVF depends on patient preference and specific medical conditions. In select groups of patients (under the age of 35, normal ovarian reserve) pregnancy success rates for Mini IVF treatment is excellent, if not higher than with traditional IVF. Women of all reproductive ages with reduced ovarian reserve often produce a lower number of eggs irrespective of the stimulation dose and may benefit from Mini-IVF as well. Some patients over 40 years of age may specifically benefit from Mini-IVF if traditional IVF had previously resulted in poor quality embryos since the gentler stimulation of Mini IVF may be less damaging to eggs and may yield better quality embryos.
At CCRH we specialize in Mini IVF protocols that are safe, proven, effective, and highly affordable. A comprehensive consultation with us will help determine if you are a good candidate for Mini IVF.
CCRH IVF Success Rates
The California Center for Reproductive Health has consistently delivered high IVF success rates, exceeding national averages in practically all age groups. Cumulative live birth rates for 2021 (the latest reporting year) are featured below:

Don’t just take our word for it!
Listen to what our patients have to say.

3,000+

20+

2X
Other Fertility Treatments You Might Consider
Our Locations
Choose your preferred location
FAQ
What does a reproductive endocrinologist and infertility specialist do?
Reproductive endocrinology and Infertility is a sub-specialty of Obstetrics and Gynecology. In addition to managing medical and surgical treatment of disorders of the female reproductive tract, reproductive endocrinologist and infertility (REI) specialists undergo additional years of training to provide fertility treatments using assisted reproductive technology (ART) such as in vitro fertilization.
Reproductive endocrinologists receive board certification by the American Board of Obstetrics and Gynecology in both Obstetrics and Gynecology and Reproductive Endocrinology and Infertility.
When should I see an REI specialist?
In general, patients should consider consulting with an REI specialist after one year of trying unsuccessfully to achieve pregnancy. The chance of conceiving every month is around 20%, therefore after a full year of trying approximately 15% of couples will still not have achieved a pregnancy.
However, if a woman is over the age of 35 it would be reasonable to see a fertility specialist earlier, typically after 6 months of trying.
Other candidates to seek earlier treatment are women who have irregular menses, endometriosis, fibroids, polycystic ovary syndrome (PCOS), women who have had 2 or more miscarriages, or problems with the fallopian tubes (prior ectopic pregnancy).
What are the reasons we are having trouble conceiving?
Approximately 1/3 of the time cause for infertility is a female factor, 1/3 of the time a male factor, and the remaining 1/3 a couples’ factor.
At CCRH, we emphasize the importance of establishing a correct diagnosis. Both partners undergo a comprehensive evaluation including a medical history and physical exam.
Furthremore, the woman’s ovarian reserve is assessed with a pelvic ultrasound and a hormonal profile. A hysterosalpingogram (HSG) will confirm fallopian tube patency and the uterine cavity is free of intracavitary lesions. A semen analysis is also obtained to evaluate for concentration, motility, and morphology of the sperm.
Additional work up is then individualized to direct the best possible treatment option for each couple.
What is IVF? What is the process like?
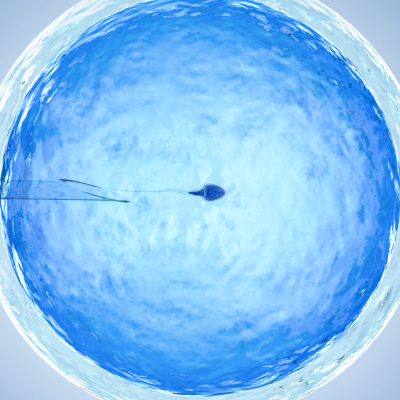
In vitro fertilization (IVF) is the process that involves fertilization of an egg outside of a woman’s body.
The process starts with fertility drugs prescribed to help stimulate egg development. In your natural cycle, your body is only able to grow one dominant egg, but with stimulation medication we can recruit multiple eggs to continue to grow. After about 8-10 days of stimulation, the eggs are surgically retrieved and then fertilized with sperm in a specialized laboratory. Fertilized eggs are then cultured under a strictly controlled environment within specialized incubators in the IVF laboratory for 3-5 days while they develop as embryos. Finally, embryos (or an embryo) are transferred into the uterine cavity for implantation.
Should I have IVF?
Before deciding if IVF is the right choice, it’s important to sit down with an REI specialist to discuss available treatment options. For some people, other methods such as fertility drugs, intrauterine insemination (IUI) may be the best first choice treatment. At CCRH, we believe each individual couple is unique and not everyone needs IVF.
Is the IVF procedure painful?
While not painful, the fertility medications may some side effects including headaches, hot flashes, mood swings, and bloating. The injection sites may also bruise.
Will IVF guarantee a baby?
Unfortunately, no. Many people think once they start IVF it’s a matter of time that they will be pregnant and have a baby. But according to national statistics per the Society of Assisted Reproduction (SART), on average 40% of assisted reproduction cycles achieve live births in women under age 35. The chances of success then continue to decrease with advancing age.
At CCRH, we employ only evidence-based interventions to ensure patient safety and optimal outcome. While we cannot guarantee a baby, we guarantee that you will receive the best, most advanced, personalized care to help you maximize your chance of a baby.
What is the success rate for IVF?
The average IVF success rate (success measured in live birth rate) using one’s own eggs begins to drop around age 35 and then rapidly after age 40. This is due to the decline in egg quantity and egg quality as a woman ages.
Our clinic’s success rate consistently beats the national average year after year.
Do insurance plans cover infertility treatment? How much does IVF cost?
Individual insurance plans often do not have any coverage for infertility treatments. If you have a group plan, you can call members services to see if they have coverage for infertility (including consultation/workup and IVF).
After your consultation with our REI specialist, one of our dedicated account managers with sit with you to go over the cost of treatment.