Freeze-All Embryo Transfer / IVF
In-vitro fertilization and embryo freeze-all (IVF-freeze-all) involves creating embryos in a standard IVF process but freezing of all embryos so that a fresh embryo transfer into the uterus, which is normally performed within five days of the egg retrieval, is avoided. Multiple indications for embryo freeze-all exist, including a suboptimal (non-receptive) uterine lining, the finding of a uterine lesion which may hinder implantation of embryos (i.e. uterine polyp, fibroid, or scarring), concerns for ovarian hyperstimulation syndrome (OHSS) which may be exacerbated by the transfer of fresh embryos, the employment of preimplantation genetic testing (PGT) for embryo chromosome screening, and diminished uterine receptivity/increased risk for embryo implantation failure which may occur under certain IVF clinical conditions more common with fresh embryo transfers.
With exceptionally reliable embryo freezing techniques used in modern IVF laboratories, embryo freeze-all has revolutionized IVF care and success rates, allowing great flexibility and optimization of IVF treatment, which no longer relies on fresh embryo transfers to achieve pregnancy under suboptimal conditions. In fact, under certain clinical conditions, assisted reproductive techniques (ART) using frozen embryos yield superior pregnancy and live birth rates than those achieved with fresh embryos.
When an indication exists for embryo freeze-all, the IVF treatment is divided into two separate but equally important treatment cycles: the IVF-freeze-all cycle, and the frozen embryo transfer (FET) cycle. The freezing of all embryos resulting from the IVF cycle allows time for the correction of uterine factors associated with implantation failure, before an embryo transfer is finally done. For instance, if the uterine lining during the ovarian stimulation phase of the IVF treatment is inadequately thick for ideal receptivity of an embryo, this can be corrected during an FET cycle before a frozen-thawed embryo is implanted, thereby optimizing implantation rates. In the case of a diagnosed uterine polyp or fibroid or intrauterine scarring (intrauterine adhesions leading to Asherman’s syndrome), known to hinder implantation of an embryo, the IVF cycle can still proceed without delay and an embryo freeze-all is performed; after which surgical correction of the lesion is performed to normalize the uterine cavity, followed by an FET cycle and the transfer of a frozen-thawed embryo into a more receptive uterine environment.
Embryo freeze-all is particularly important for patients of advanced maternal age and/or those with diminished ovarian reserve where a delay in initiating IVF (and creating embryos), due to the need for surgery, for instance, may be detrimental to IVF success. Since the time span between the IVF-embryo freeze-all cycle and the subsequent FET cycle does not negatively impact ART success rates, patients can be rest assured that clinically indicated embryo freezing followed by a delay in initiating an FET cycle will improve rather than decrease their ART success rates.
A common indication for embryo freeze-all following IVF is elevated hormone levels often reached during the IVF stimulation treatment. In particular, estrogen and/or progesterone levels, which exceed certain threshold levels, are associated with an increased risk for embryo implantation failure when fresh embryos are transferred into the uterus within five days of the egg retrieval procedure. In contrast, since ovarian stimulation is uncommon during the majority of FET cycles, estrogen and progesterone levels typically remain low during FETs, simulating a natural cycle, and therefore allowing frozen-thawed embryos to be transferred into a more receptive uterine environment, resulting in superior outcomes. In addition to improved implantation and live birth rates resulting from frozen embryo transfers, FET cycles are associated with lower miscarriage rates, a lower risk of preterm labor, and a possible lower risk for ectopic pregnancies as compared with fresh embryo transfers.
Don’t just take our word for it!
Listen to what our patients have to say.

3,000+

20+

2X
FAQ
Reproductive endocrinology and Infertility is a sub-specialty of Obstetrics and Gynecology. In addition to managing medical and surgical treatment of disorders of the female reproductive tract, reproductive endocrinologist and infertility (REI) specialists undergo additional years of training to provide fertility treatments using assisted reproductive technology (ART) such as in vitro fertilization.
Reproductive endocrinologists receive board certification by the American Board of Obstetrics and Gynecology in both Obstetrics and Gynecology and Reproductive Endocrinology and Infertility.
In general, patients should consider consulting with an REI specialist after one year of trying unsuccessfully to achieve pregnancy. The chance of conceiving every month is around 20%, therefore after a full year of trying approximately 15% of couples will still not have achieved a pregnancy.
However, if a woman is over the age of 35 it would be reasonable to see a fertility specialist earlier, typically after 6 months of trying.
Other candidates to seek earlier treatment are women who have irregular menses, endometriosis, fibroids, polycystic ovary syndrome (PCOS), women who have had 2 or more miscarriages, or problems with the fallopian tubes (prior ectopic pregnancy).
Approximately 1/3 of the time cause for infertility is a female factor, 1/3 of the time a male factor, and the remaining 1/3 a couples’ factor.
At CCRH, we emphasize the importance of establishing a correct diagnosis. Both partners undergo a comprehensive evaluation including a medical history and physical exam.
Furthremore, the woman’s ovarian reserve is assessed with a pelvic ultrasound and a hormonal profile. A hysterosalpingogram (HSG) will confirm fallopian tube patency and the uterine cavity is free of intracavitary lesions. A semen analysis is also obtained to evaluate for concentration, motility, and morphology of the sperm.
Additional work up is then individualized to direct the best possible treatment option for each couple.
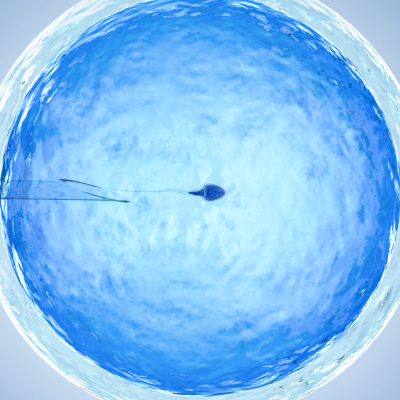
In vitro fertilization (IVF) is the process that involves fertilization of an egg outside of a woman’s body.
The process starts with fertility drugs prescribed to help stimulate egg development. In your natural cycle, your body is only able to grow one dominant egg, but with stimulation medication we can recruit multiple eggs to continue to grow. After about 8-10 days of stimulation, the eggs are surgically retrieved and then fertilized with sperm in a specialized laboratory. Fertilized eggs are then cultured under a strictly controlled environment within specialized incubators in the IVF laboratory for 3-5 days while they develop as embryos. Finally, embryos (or an embryo) are transferred into the uterine cavity for implantation.
Before deciding if IVF is the right choice, it’s important to sit down with an REI specialist to discuss available treatment options. For some people, other methods such as fertility drugs, intrauterine insemination (IUI) may be the best first choice treatment. At CCRH, we believe each individual couple is unique and not everyone needs IVF.
While not painful, the fertility medications may some side effects including headaches, hot flashes, mood swings, and bloating. The injection sites may also bruise.
Unfortunately, no. Many people think once they start IVF it’s a matter of time that they will be pregnant and have a baby. But according to national statistics per the Society of Assisted Reproduction (SART), on average 40% of assisted reproduction cycles achieve live births in women under age 35. The chances of success then continue to decrease with advancing age.
At CCRH, we employ only evidence-based interventions to ensure patient safety and optimal outcome. While we cannot guarantee a baby, we guarantee that you will receive the best, most advanced, personalized care to help you maximize your chance of a baby.
The average IVF success rate (success measured in live birth rate) using one’s own eggs begins to drop around age 35 and then rapidly after age 40. This is due to the decline in egg quantity and egg quality as a woman ages.
Our clinic’s success rate consistently beats the national average year after year.
Individual insurance plans often do not have any coverage for infertility treatments. If you have a group plan, you can call members services to see if they have coverage for infertility (including consultation/workup and IVF).
After your consultation with our REI specialist, one of our dedicated account managers with sit with you to go over the cost of treatment.