Low Responder IVF: What It Means and How It Can Help You Conceive

For many women and couples trying to conceive, the journey can feel like an emotional rollercoaster. If you’ve undergone fertility testing or treatment and been told you’re a “low responder,” it’s understandable to feel discouraged. But being a low responder during IVF doesn’t mean your dream of having a baby is out of reach. With the right protocol and expert guidance in reproductive medicine, there is still hope.
In this guide, we’ll walk you through what it means to be a low responder, what causes a poor ovarian response, and the options available that are designed specifically for IVF poor responders.
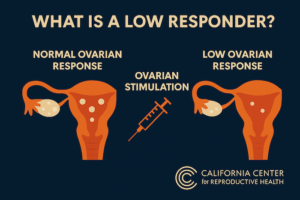
What Is a Low Responder in IVF?
Medical Definition of a Low Responder
A “low responder” in IVF refers to someone whose ovaries produce fewer eggs than expected in response to ovarian stimulation. This is often diagnosed during or after an IVF cycle, when the number of oocytes retrieved is lower than anticipated.
Clinically, the ESHRE Bologna criteria define poor responders as patients meeting at least two of the following:
- Advanced maternal age (≥40 years).
- Previous poor ovarian response (≤3 oocytes with conventional stimulation).
- Abnormal ovarian reserve tests (e.g., low AMH or low antral follicle count).
Common Indicators and Risk Factors
Several factors can contribute to a poor response during IVF:
- Advanced maternal age: Egg quantity and quality decline with age.
- Low ovarian reserve: Often measured via AMH levels, antral follicle count, or FSH levels.
- Previous ovarian surgery: Can reduce ovarian tissue and blood flow.
- Genetic predispositions or autoimmune conditions.
- Lifestyle factors: Smoking, stress, or being underweight/overweight.
Emotional Toll on Patients
Being labeled a poor responder can feel like a heavy blow, especially after months or years of trying to conceive. The emotional toll includes anxiety, frustration, and fear that treatment may not work. However, it’s important to remember that a poor response doesn’t equal no chance. Many women in this category have gone on to have successful pregnancies with personalized care and the right approach in reproductive medicine.
Why Does a Low Ovarian Response Happen?
Role of Hormones in Follicular Development
During a typical IVF cycle, medications stimulate the ovaries to produce multiple eggs. These medications often include gonadotropins, which contain follicle stimulating hormone (FSH) and luteinizing hormone (LH).
Poor ovarian responders may have:
- Ovaries that don’t respond adequately to ovarian stimulation.
- Hormonal imbalances that impair follicle development.
- A limited number of follicles to begin with.
Low Ovarian Reserve vs. Ovarian Failure
While these terms are sometimes used interchangeably, they describe different scenarios:
- Low ovarian reserve: Fewer eggs available, but still capable of producing a response with the right stimulation strategy.
- Ovarian failure: Complete loss of ovarian function, usually requiring donor eggs.
Understanding the difference is crucial for choosing the right fertility treatment.
IVF Options for Poor Responders
Ovarian Stimulation Protocols Tailored for Poor Responders
| Protocol Type | Medication Dose | Cycle Duration | Typical Candidates | Pros | Cons |
|---|---|---|---|---|---|
| Mild Stimulation | Low dose gonadotropins + oral agents (e.g. letrozole, clomiphene) | Shorter (8–10 days) | Poor responders, advanced maternal age, or those with low ovarian reserve | Lower medication cost, reduced risk of ovarian hyperstimulation | Fewer oocytes retrieved, potentially lower cumulative success |
| Conventional Stimulation | High dose gonadotropins (FSH, LH) | 10–14 days | Patients with normal ovarian reserve or unknown prognosis | Higher oocyte yield, higher chance of embryos per cycle | Higher cost, risk of ovarian hyperstimulation, more side effects |
| Antagonist Protocol | Flexible gonadotropin dose + GnRH antagonist | 8–12 days | Poor responders or those at risk of poor response or early LH surge | Personalized dosing, shorter cycle, better control over LH surge | Requires close monitoring, response still may be suboptimal |
For women diagnosed as low responders, choosing the right stimulation protocol is essential. Some of the most effective approaches include:
- Antagonist protocol is flexible protocol that allows lower hormone doses while preventing premature ovulation – often used for poor responders who need a gentler, more adaptive approach. This strategy has been shown to be particularly effective in patients with poor ovarian reserve.
- Microdose flare protocol uses low doses of GnRH agonists to stimulate a stronger response in ovaries that are otherwise less responsive.
- DuoStim (dual stimulation) stimulates the ovaries twice in one menstrual cycle (follicular and luteal phase), increasing the number of eggs retrieved in a shorter time frame. A recent study found this method significantly increased the egg yield in low responder patients.
Conventional vs. Mild Stimulation: Which Works Best?
Conventional stimulation uses higher doses of gonadotropins, aiming to retrieve as many eggs as possible. However, in poor responders, this doesn’t always lead to better outcomes and can increase the risk of ovarian hyperstimulation.
According to a guideline published by the ASRM, mild ovarian stimulation protocols in poor responders can offer similar pregnancy rates compared to conventional high-dose approaches, but with lower cost and less stress on the body.
The Importance of Personalization in Treatment
No two patients are the same, and for poor responders, personalization is key. Fertility clinics may now use:
- AI-driven stimulation planning to predict the best protocol for each ovarian stimulation cycle.
- Pharmacogenomic testing to assess how patients metabolize fertility drugs.
- Detailed hormonal profiling to improve response to ovarian stimulation.
A 2014 study emphasized the importance of tailoring treatment based on individual hormonal and ovarian reserve profiles to improve outcomes in poor responders. The goal is to create a protocol tailored to your body’s unique hormone levels and reproductive goals.
Success Rates and What to Expect
How Many Eggs Are Enough?
While typical IVF cycles aim for 10-15 eggs, success is still possible with fewer:
- Studies show that even 1-2 high-quality embryos can result in pregnancy.
- Quality matters more than quantity, especially for women with diminished reserves.

Success Rates for Poor Responders Undergoing IVF
Success rates vary based on age, low ovarian response, and the stimulation protocol used:
- Women under 35 with a poor response may still see promising outcomes.
- For those over 40 with poor ovarian reserve, success may require multiple IVF treatments or alternative strategies such as egg donation.
The key takeaway is that poor ovarian response doesn’t mean zero chance – it just means a different approach may be necessary.
Emotional and Financial Considerations
Poor responders often face a higher emotional and financial burden due to:
- The possibility of multiple IVF treatments.
- Lower success per cycle.
- Limited or no insurance coverage.
Support from a fertility counselor and a clear financial plan can help manage the journey. Some clinics offer multi-cycle discount packages or refund programs tailored for poor responders.
Complementary and Alternative Approaches
Supplements and Nutritional Support
Several supplements may help improve egg quality and ovarian response:
- DHEA: May support androgen levels and increase follicle count.
- CoQ10: Enhances mitochondrial function in eggs.
- Antioxidants: Protect egg cells from oxidative stress.
Always consult your fertility doctor before starting supplements.
Lifestyle Changes to Improve Ovarian Response
Simple lifestyle adjustments may enhance fertility outcomes:
- Adopt a Mediterranean-style diet rich in whole grains, healthy fats, and lean proteins.
- Reduce alcohol and caffeine intake.
- Prioritize sleep and stress management.
- Maintain a healthy weight through moderate exercise.
These changes support overall hormonal balance and reproductive health.
When to Consider Other Fertility Treatments
When IVF Isn’t Enough
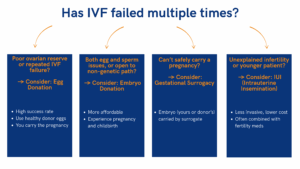
In cases where multiple IVF attempts fail, your doctor may suggest alternative paths:
- Egg donation: For women with extremely poor ovarian reserve, ovarian failure, or repeated IVF failure, egg donation offers one of the highest success rates in assisted reproductive technology. Donor eggs come from healthy, screened women (usually under 30) and are fertilized with your partner’s or donor sperm, then transferred to your uterus. While emotionally complex, this option allows for pregnancy, childbirth, and the early nurturing bond with your child.
- Embryo donation: This involves adopting surplus embryos from another couple’s IVF. It can be more affordable than egg donation and allows patients to experience pregnancy and birth, even if the genetic link isn’t present. Embryo donation is ideal for couples facing both egg and sperm-related challenges or for those open to alternative family-building paths.
- Gestational surrogacy: In cases of repeated implantation failure, uterine abnormalities, or medical conditions preventing safe pregnancy, gestational surrogacy may be recommended. Your embryo (created with your egg or a donor’s) is transferred to a surrogate’s uterus, allowing you to become a parent when carrying the pregnancy isn’t possible.
- Intrauterine insemination (IUI): For select low responder patients with regular ovulation and open fallopian tubes, intrauterine insemination may be considered before IVF. While IUI typically has lower success rates than IVF, it can be combined with gonadotropin stimulation to enhance follicle development and improve the odds of conception in younger patients or those with unexplained infertility.
While these options may be emotionally difficult, they offer excellent success rates and the opportunity to build a family.
Navigating Complex Reproductive Decisions
Choosing the next step can be overwhelming. Many couples benefit from:
- Fertility counseling.
- Second opinions from reproductive endocrinologists.
- Support groups or online communities.
Being informed and supported empowers you to make the best decisions for your journey to parenthood.
Start Your Personalized IVF Plan with Experts Who Understand Low Responders
Facing a low ovarian response or being labeled a poor responder can be overwhelming – but it doesn’t mean your journey to parenthood is over. Advances in reproductive medicine, personalized ovarian stimulation protocols, and evolving approaches like antagonist protocols and gonadotropin stimulation are improving outcomes every year.
If you’re struggling with fertility and wondering which approach is right for you, our clinic specializes in treating low response patients. Let’s find a treatment plan tailored to your unique biology and fertility goals. Schedule a consultation with our fertility specialists today and take the next step toward building your family with confidence!
Eliran Mor, MD
Reproductive Endocrinologist located in Encino, Santa Monica, Valencia & West Hollywood, CA
FAQ
What does a reproductive endocrinologist and infertility specialist do?
Reproductive endocrinology and Infertility is a sub-specialty of Obstetrics and Gynecology. In addition to managing medical and surgical treatment of disorders of the female reproductive tract, reproductive endocrinologist and infertility (REI) specialists undergo additional years of training to provide fertility treatments using assisted reproductive technology (ART) such as in vitro fertilization.
Reproductive endocrinologists receive board certification by the American Board of Obstetrics and Gynecology in both Obstetrics and Gynecology and Reproductive Endocrinology and Infertility.
When should I see an REI specialist?
In general, patients should consider consulting with an REI specialist after one year of trying unsuccessfully to achieve pregnancy. The chance of conceiving every month is around 20%, therefore after a full year of trying approximately 15% of couples will still not have achieved a pregnancy.
However, if a woman is over the age of 35 it would be reasonable to see a fertility specialist earlier, typically after 6 months of trying.
Other candidates to seek earlier treatment are women who have irregular menses, endometriosis, fibroids, polycystic ovary syndrome (PCOS), women who have had 2 or more miscarriages, or problems with the fallopian tubes (prior ectopic pregnancy).
What are the reasons we are having trouble conceiving?
Approximately 1/3 of the time cause for infertility is a female factor, 1/3 of the time a male factor, and the remaining 1/3 a couples’ factor.
At CCRH, we emphasize the importance of establishing a correct diagnosis. Both partners undergo a comprehensive evaluation including a medical history and physical exam.
Furthremore, the woman’s ovarian reserve is assessed with a pelvic ultrasound and a hormonal profile. A hysterosalpingogram (HSG) will confirm fallopian tube patency and the uterine cavity is free of intracavitary lesions. A semen analysis is also obtained to evaluate for concentration, motility, and morphology of the sperm.
Additional work up is then individualized to direct the best possible treatment option for each couple.
What is IVF? What is the process like?
In vitro fertilization (IVF) is the process that involves fertilization of an egg outside of a woman’s body.
The process starts with fertility drugs prescribed to help stimulate egg development. In your natural cycle, your body is only able to grow one dominant egg, but with stimulation medication we can recruit multiple eggs to continue to grow. After about 8-10 days of stimulation, the eggs are surgically retrieved and then fertilized with sperm in a specialized laboratory. Fertilized eggs are then cultured under a strictly controlled environment within specialized incubators in the IVF laboratory for 3-5 days while they develop as embryos. Finally, embryos (or an embryo) are transferred into the uterine cavity for implantation.
Should I have IVF?
Before deciding if IVF is the right choice, it’s important to sit down with an REI specialist to discuss available treatment options. For some people, other methods such as fertility drugs, intrauterine insemination (IUI) may be the best first choice treatment. At CCRH, we believe each individual couple is unique and not everyone needs IVF.
Is the IVF procedure painful?
While not painful, the fertility medications may some side effects including headaches, hot flashes, mood swings, and bloating. The injection sites may also bruise.
Will IVF guarantee a baby?
Unfortunately, no. Many people think once they start IVF it’s a matter of time that they will be pregnant and have a baby. But according to national statistics per the Society of Assisted Reproduction (SART), on average 40% of assisted reproduction cycles achieve live births in women under age 35. The chances of success then continue to decrease with advancing age.
At CCRH, we employ only evidence-based interventions to ensure patient safety and optimal outcome. While we cannot guarantee a baby, we guarantee that you will receive the best, most advanced, personalized care to help you maximize your chance of a baby.
What is the success rate for IVF?
The average IVF success rate (success measured in live birth rate) using one’s own eggs begins to drop around age 35 and then rapidly after age 40. This is due to the decline in egg quantity and egg quality as a woman ages.
Our clinic’s success rate consistently beats the national average year after year.
Do insurance plans cover infertility treatment? How much does IVF cost?
Individual insurance plans often do not have any coverage for infertility treatments. If you have a group plan, you can call members services to see if they have coverage for infertility (including consultation/workup and IVF).
After your consultation with our REI specialist, one of our dedicated account managers with sit with you to go over the cost of treatment.






