What Most People Don’t Know About Infertility
Infertility means a woman can’t get pregnant after a full year of dedicated trying, or six months if the woman is 35 or older. If you’re struggling to stay pregnant, you may also be diagnosed with infertility.
At California Center for Reproductive Health, our specialists have treated thousands of women, men, and couples struggling with infertility. Many of these patients come in without a full understanding of what it means to be infertile.
Here’s what we want you to know about infertility.
Getting pregnant isn’t easy
When you’re trying to get pregnant, it seems like everyone is having an easy time of it — except you. The truth is: Getting pregnant is a complex process. Many steps have to play out just right for a couple to create a pregnancy:
- The woman must be able to produce and release an egg from her ovaries
- The egg must have a clear path through the fallopian tubes toward the uterus
- The man’s sperm must be healthy and be able to meet the egg along the way
- The fertilized egg has to successfully attach to the inside of the uterus
Multiple problems can happen with any of these steps, preventing conception and causing infertility.
It’s not always the woman’s issue
Often, a woman who has trouble conceiving blames herself. But, infertility can be a result of problems with the man or combined problems in a couple. Only one-third of infertility cases are caused by women’s problems.
Another third of infertility cases are due to problems with the man’s body or sperm quality. The last third of infertility cases are caused by unknown problems or a combination of issues with the man and woman.
Women may be infertile due to untreated chlamydia or gonorrhea, failure to ovulate, blockages in the fallopian tubes, poor egg quality, uterine irregularities, endometriosis, or uterine fibroids.
Common reasons a man may struggle with infertility include untreated chlamydia or gonorrhea, low sperm count or poor sperm motility, irregularly formed sperm, thick semen, or a lack of sperm altogether.
Infertility isn’t only the inability to conceive
Recurrent pregnancy loss is also considered a form of infertility. We offer comprehensive work-ups if you’ve experienced two or more first trimester miscarriages or one or more second trimester miscarriages.
Losing a pregnancy is devastating, and we also offer counseling and support to help you through your grief. Be comforted, though, that in the vast majority of cases, we can offer treatments that greatly reduce your risk of having another miscarriage.
Infertility is common
About one in every six couples has trouble getting pregnant or staying pregnant. More than 7.4 million women have received infertility services in their lifetimes. About 10% of all males in the United States who are trying to conceive suffer from infertility.
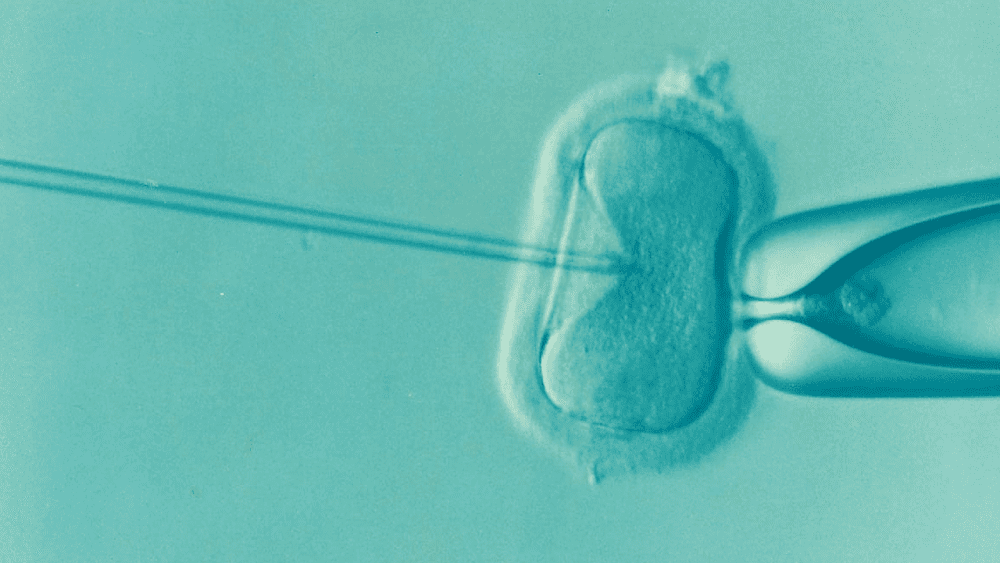
We work with you to identify the reason for your trouble conceiving and offer real solutions, including IVF and embryo transfer.
Age matters
When a woman waits until after age 35 to try to have children, it can be a factor in fertility problems. As a woman gets older, her ovaries are l
Miscarriages are more common in women older than 35, and health problems that cause complications for pregnancy are more common in this age group.
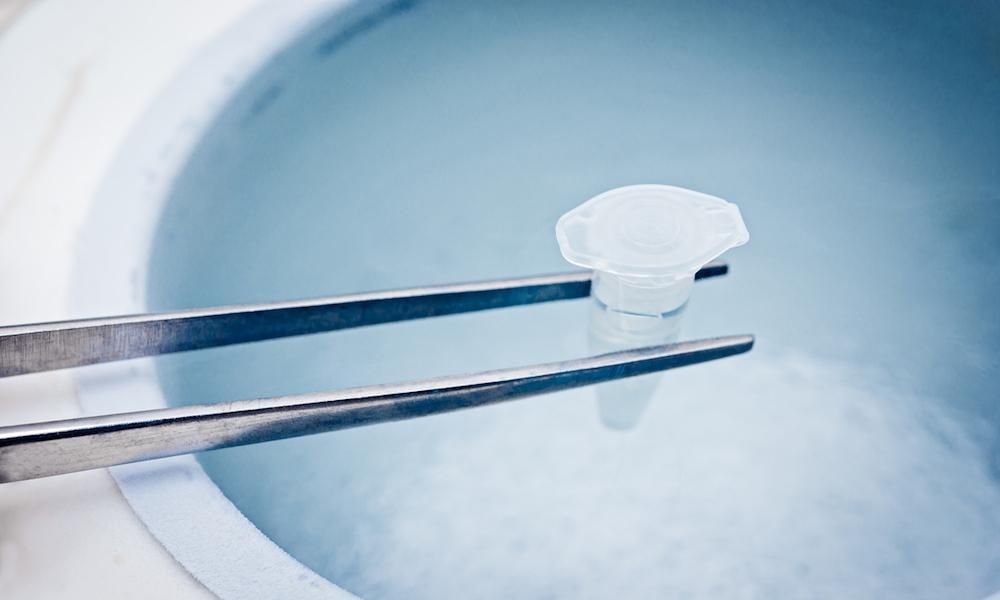
At California Center for Reproductive Health, we understand that life doesn’t always cooperate with your biological fertility timeline. We can help with egg freezing, egg donation, embryo freezing, surrogacy, artificial insemination, and other solutions to your infertility.
If you’re struggling with infertility, solutions are available. We support couples’ infertility journeys and help them go on to have healthy pregnancies.
Call one of our offices in Encino, Alhambra, Valencia, or West Hollywood, or use this website to request a consultation. Our compassionate team helps you determine the best way to overcome infertility and create your family.