Egg Freezing vs. Embryo Freezing: Which is Right for You?
In vitro fertilization, or IVF, is on the rise. How popular is this healthcare decision? MarketsandMarkets projects it will expand to more than three-quarters of a billion dollars, $756.7 million, by 2021. Even in 2016, the industry was already measuring nearly a half-billion at $468.3 million. Assuming that the forecast is accurate, that would mean the compound annual growth rate (CAGR) would be 10.1%. There are various reasons for this increase: dropping fertility rates, more instances of male infertility, and a rise in the average time that a woman first becomes a mother, etc.
As in vitro fertilization has become more prevalent, so have egg or embryo freezing – also called cryopreservation. Are you considering these procedures, but you aren’t quite sure on the details of what they are? If so, we can help. Let’s look at each one in isolation – what they are exactly, and what steps are involved with a healthcare clinic – and then explore why someone might choose one over the other. Before that, though, let’s ground ourselves by briefly discussing in vitro fertilization.
- In vitro fertilization
- Egg freezing
- Embryo freezing
- 3 questions to help you choose egg freezing or embryo freezing
- The right healthcare for a healthy baby
In vitro fertilization
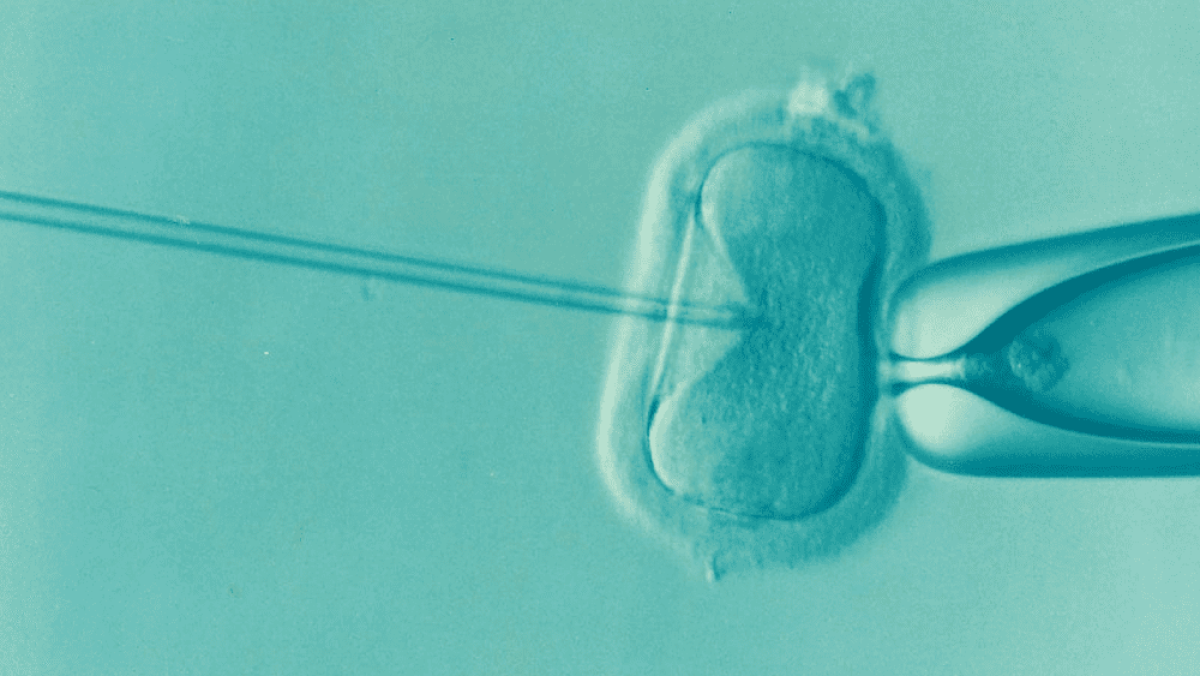
In 1978, Louise Brown of England became the first baby to be conceived outside of a mother’s womb. In that role, she was the first IVF success story. When people think of IVF, it is often confused with artificial insemination — but that process means that conception is normal and the only difference is the placement of sperm into the uterus. IVF is different because the technique, the combination of the sperm and egg, occurs in a lab setting. Note that embryos are reintroduced, implanted into the uterus, once they have initially grown outside the body.
Egg freezing
Egg freezing, technically called mature oocyte cryopreservation, is a way that women can retain their reproductive capability. In the process, a specialist harvests eggs from your ovaries. They are then frozen in the absence of fertilization and put into storage to be utilized at some point in the future.
Now let’s jump forward in time. You can thaw an egg that has been frozen in this manner, introduce it to sperm under laboratory conditions, and implant it into the uterus. In other words, IVF can be used at a later date to reintroduce the egg to your body.
Eliran Mor, MD
Reproductive Endocrinologist located in Encino, Santa Monica, Valencia & West Hollywood, CA
FAQ
Reproductive endocrinology and Infertility is a sub-specialty of Obstetrics and Gynecology. In addition to managing medical and surgical treatment of disorders of the female reproductive tract, reproductive endocrinologist and infertility (REI) specialists undergo additional years of training to provide fertility treatments using assisted reproductive technology (ART) such as in vitro fertilization.
Reproductive endocrinologists receive board certification by the American Board of Obstetrics and Gynecology in both Obstetrics and Gynecology and Reproductive Endocrinology and Infertility.
In general, patients should consider consulting with an REI specialist after one year of trying unsuccessfully to achieve pregnancy. The chance of conceiving every month is around 20%, therefore after a full year of trying approximately 15% of couples will still not have achieved a pregnancy.
However, if a woman is over the age of 35 it would be reasonable to see a fertility specialist earlier, typically after 6 months of trying.
Other candidates to seek earlier treatment are women who have irregular menses, endometriosis, fibroids, polycystic ovary syndrome (PCOS), women who have had 2 or more miscarriages, or problems with the fallopian tubes (prior ectopic pregnancy).
Approximately 1/3 of the time cause for infertility is a female factor, 1/3 of the time a male factor, and the remaining 1/3 a couples’ factor.
At CCRH, we emphasize the importance of establishing a correct diagnosis. Both partners undergo a comprehensive evaluation including a medical history and physical exam.
Furthremore, the woman’s ovarian reserve is assessed with a pelvic ultrasound and a hormonal profile. A hysterosalpingogram (HSG) will confirm fallopian tube patency and the uterine cavity is free of intracavitary lesions. A semen analysis is also obtained to evaluate for concentration, motility, and morphology of the sperm.
Additional work up is then individualized to direct the best possible treatment option for each couple.
In vitro fertilization (IVF) is the process that involves fertilization of an egg outside of a woman’s body.
The process starts with fertility drugs prescribed to help stimulate egg development. In your natural cycle, your body is only able to grow one dominant egg, but with stimulation medication we can recruit multiple eggs to continue to grow. After about 8-10 days of stimulation, the eggs are surgically retrieved and then fertilized with sperm in a specialized laboratory. Fertilized eggs are then cultured under a strictly controlled environment within specialized incubators in the IVF laboratory for 3-5 days while they develop as embryos. Finally, embryos (or an embryo) are transferred into the uterine cavity for implantation.
Before deciding if IVF is the right choice, it’s important to sit down with an REI specialist to discuss available treatment options. For some people, other methods such as fertility drugs, intrauterine insemination (IUI) may be the best first choice treatment. At CCRH, we believe each individual couple is unique and not everyone needs IVF.
While not painful, the fertility medications may some side effects including headaches, hot flashes, mood swings, and bloating. The injection sites may also bruise.
Unfortunately, no. Many people think once they start IVF it’s a matter of time that they will be pregnant and have a baby. But according to national statistics per the Society of Assisted Reproduction (SART), on average 40% of assisted reproduction cycles achieve live births in women under age 35. The chances of success then continue to decrease with advancing age.
At CCRH, we employ only evidence-based interventions to ensure patient safety and optimal outcome. While we cannot guarantee a baby, we guarantee that you will receive the best, most advanced, personalized care to help you maximize your chance of a baby.
The average IVF success rate (success measured in live birth rate) using one’s own eggs begins to drop around age 35 and then rapidly after age 40. This is due to the decline in egg quantity and egg quality as a woman ages.
Our clinic’s success rate consistently beats the national average year after year.
Individual insurance plans often do not have any coverage for infertility treatments. If you have a group plan, you can call members services to see if they have coverage for infertility (including consultation/workup and IVF).
After your consultation with our REI specialist, one of our dedicated account managers with sit with you to go over the cost of treatment.




