Reciprocal IVF Cost: Complete Price Breakdown for Same-Sex Female Couples [2026]
Let’s talk money. Not because it’s fun (it’s not), but because family building through reciprocal IVF is probably one of the biggest financial commitments you’ll make together, and you deserve to know exactly what you’re getting into.
How CCRH Compares: High Success Rates, LGBTQ+ Expertise, and Lower Costs
At the California Center for Reproductive Health (CCRH), we specialize in reciprocal IVF for same-sex female couples — and our pricing is typically lower than most fertility clinics in Los Angeles and across California. While many clinics charge $25,000–$35,000 or more per cycle, CCRH’s all-inclusive Access IVF program and in-house lab capabilities help keep costs transparent and affordable without compromising results. Led by board-certified fertility specialist Dr. Eliran Mor, our clinic combines advanced technology, individualized care, and extensive LGBTQ+ family-building experience. Couples choose CCRH not only for our proven success rates, but because they know their care — and their budget — are in the best hands.
Learn more about our Access IVF program here.
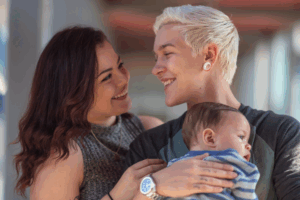
Reciprocal IVF is the IVF process where one partner provides the eggs while the other partner carries the pregnancy. It’s collaborative, intimate, and yes, it costs money.
Generally speaking, expect to pay $20,000 to $35,000+ per reciprocal IVF cycle for a baseline IVF cycle. With meds, sperm donor fees, testing, and possible frozen embryo transfer (FET) cycles, most couples budget $50,000-$70,000 for a realistic path to a baby.
This guide breaks down the cost of reciprocal IVF, insurance realities, financing, and whether reciprocal IVF is worth it for same sex female couples building a family.
Total Reciprocal IVF Cost (What You’ll Actually Pay)
Average Cost Per Cycle Breakdown
| Cost Component | Price Range |
|---|---|
| Base IVF cycle fees | $8,000-$11,000 |
| Fertility medications (both partners) | $3,500-$8,000 |
| Donor sperm | $1,000-$3,000 (2-4 vials) |
| Fertility testing & monitoring | $2,000-$4,000 |
| Additional procedures (PGT, FET) | $3,000-$7,000 |
Clinics advertise a base in vitro fertilization price that usually covers egg retrieval, the fertilization process, embryo culture, and one fresh embryo transfer. Fertility medications, ICSI, preimplantation genetic testing, donor sperm fees, anesthesia, and frozen embryos storage are usually extra. Ask your chosen fertility clinic for a line-item quote, because that’s the only honest comparison.
The Reality Check: How Many Cycles Will You Need?
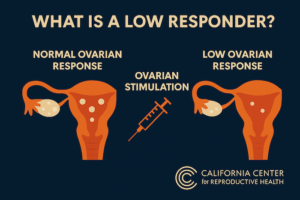
Measure cost-to-baby, not cost-per-cycle. Success per IVF cycle often sits around 40-60%, depending mainly on the age of the partner providing eggs and ovarian stimulation response.
- 1 cycle (lucky): $20k-$35k.
- 2 cycles (realistic): $40k-$70k.
- 3+ cycles: $60k-$105k+.
Plan for 2-3 IVF cycles, unless testing (AMH, AFC) suggests otherwise. That’s just smart budgeting, not pessimism.
Geographic Cost Variations
Where you go matters. Big metros (NYC, LA, SF) trend higher; mid-size cities lower. But remember IVF cost isn’t everything: success rates, LGBTQ+ experience at the clinic, and legal issues (parentage) matter for lesbian couples and family building.
Hidden Costs That Add Up Fast
Even after you budget for the basics, reciprocal IVF comes with extra expenses that can sneak up fast. Here are the most common hidden costs to plan for:
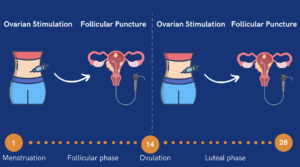
- Sync menstrual cycles (meds & monitoring): $500-$1,500.
- Canceled cycles: $3k-$8k lost.
- Double testing (both partners need labs and consults).
- Sperm vials usually cost $500-$1,200 each; needing 2-4 vials is typical.
- Travel, time off work, and mental health support.
- Infectious disease testing for both partners is mandatory.
As a rule of thumb, add a 15-20% buffer to quotes to avoid sticker shock.
Complete Cost Breakdown: Every Expense Explained
Phase 1 – Initial Consultation & Fertility Testing ($1,500-$4,000)
Both people are patients. Yes, even if only one partner will provide eggs or carry the pregnancy.
Partner A (providing eggs)
- Fertility specialist consult: $200-$500.
- Fertility testing (AMH, FSH, antral follicle count): $500-$1,000.
- Ultrasound/physical: $300-$600.
- Infectious disease testing: $200-$400.
- Genetic carrier screening (optional): $200-$500.
Partner B (carrying partner)
- Consult: $200-$500.
- Uterine evaluation (saline sonogram or hysteroscopy): $500-$1,500.
- Mock embryo transfer: $200-$500.
- Hormone testing & infectious testing: $200-$400.
This beginning treatment step confirms medical candidacy before vitro fertilization begins.
Phase 2 – Egg Retrieval & Donor Sperm ($10,000-$20,000)
This is where the bills jump.
Ovarian stimulation (Partner A)
- Fertility medications / hormonal injections: $3,000-$6,000.
- Monitoring (ultrasounds & bloodwork): $1,000-$3,000.
- Egg retrieval: $5,000-$10,000 (+ anesthesia $500-$1,000).
Expect multiple eggs retrieved: more eggs = more embryos = better chance of future siblings without repeated retrievals.
Sperm costs
- Anonymous donor via sperm bank: $500-$1,200/vial; 2-4 vials typical ($1,000-$4,800) + shipping/storage $200-$500.
- Known donor: lower per-cycle sperm costs but add legal fees ($1,000-$3,000) and required medical screening.
Phase 3 – Fertilization & Embryo Development ($5,000-$12,000)
The IVF laboratory fees and fertilization process typically range from $3,000 to $5,000. If indicated, Intracytoplasmic Sperm Injection (ICSI) can be added, costing an additional $1,500 to $3,000. Embryo culture and monitoring are usually included in the lab fees.
For couples considering Preimplantation Genetic Testing (PGT-A), the cost is roughly $3,000 to $7,000, or about $200 to $400 per embryo. PGT-A can help reduce the risk of miscarriage and failed embryo transfers. For many couples (especially when the egg provider is older), using PGT-A can ultimately lower the overall cost per successful pregnancy.
Phase 4 – Embryo Transfer & Pregnancy ($4,000-$8,000)
Preparing the uterus for embryo transfer (Partner B or carrying partner) involves medications and monitoring:
- Estrogen/progesterone medications: $500-$2,000.
- Monitoring: $500-$1,500.
Regarding transfer options:
- Fresh embryo transfer is often included in the base IVF treatment.
- Frozen embryo transfer (FET), needed if embryos are frozen or PGT was performed, typically costs $3,000-$6,000.
Pregnancy test and early monitoring generally run $200-$500.
For families planning future siblings without another retrieval, embryo or egg freezing is worth considering:
- Initial procedure: $500-$1,500.
- Storage: $300-$800 per year.
Insurance Coverage & Financing Your Reciprocal IVF Journey
Understanding Insurance Coverage for Reciprocal IVF
Insurance is inconsistent and often not designed for co IVF or reciprocal IVF. Insurers may require an infertility diagnosis, or they might code coverage differently for same sex female couples.
What’s typically covered vs. not covered
- Often covered: some fertility testing, occasionally partial fertility medications.
- Sometimes: bits of the IVF process or monitoring.
- Rarely: sperm fees, preimplantation genetic testing, and embryo storage.
States with mandatory IVF coverage
A few states mandate fertility benefits (examples: CT, IL, MD, MA, NJ, NY). But “mandated” doesn’t mean full coverage for reciprocal IVF or lesbian couples in all cases.
How to check your specific coverage
Call HR and the insurer. Ask: “Does my plan cover reciprocal IVF or partner IVF? Is an infertility diagnosis required? Are meds pharmacy or medical benefit? What’s the lifetime maximum?” Get answers in writing. If denied, appeal: clinics often help with documentation.
Employer fertility benefits (if available) can dramatically change the math. Look for $10k-$50k employer funds.
Creative Ways to Reduce Costs Without Compromising Success
Multi-cycle discount packages
Shared-risk or refund programs (prepay multiple cycles) can save 15-30% but require up-front cash and have eligibility rules.
Medication cost reduction
- Use generics when safe (30-50% savings).
- Shop specialty fertility pharmacies, big chains, or Costco.
- Manufacturer assistance / discount programs can cut meds dramatically.
- International pharmacies are a gray area, so use caution.
Known donor vs. anonymous donor
Sperm bank route costs per vial; known donor swaps per-vial fees for legal/screening costs. If you plan multiple children, buying extra vials from the same donor can be cheaper.
Strategic timing
Align with plan year, max out FSA/HSA, and schedule treatment to maximize employer benefits.
Clinical trials and research studies
Some clinics/universities subsidize IVF in exchange for participation.
What NOT to compromise on
Don’t skimp on the fertility specialist, lab quality, or LGBTQ+ experience: save on logistics and meds, not on expertise.

Financing Options and Payment Plans
Fertility clinic payment plans
Many clinics offer in-house plans or work with lenders. Compare interest, terms, and multi-cycle options.
Fertility-specific loans
Firms like Sunfish and Kindbody offer finance products tailored to fertility (typical rates 6-15%).
Traditional financing
Personal loans, HELOC, or credit cards (only if you can manage interest). 401(k) loans are a last resort.
Grants & assistance programs
Organizations such as Family Equality and the BabyQuest Foundation provide targeted grants. Local LGBTQ+ centers sometimes offer funds. Apply widely and early.
FSA/HSA advantages
Use pre-tax dollars for procedures, meds, and travel. It’s an immediate 20-30% effective saving. Note: donor sperm may not always qualify.
Crowdfunding considerations
Public, imperfect: people have success but expect modest amounts. Consider privacy and relationship dynamics.
Tax Deductions and Financial Planning
Medical expense deductions apply if medical costs exceed the IRS threshold; keep meticulous receipts, EOBs, and mileage logs. Work with a tax pro who understands fertility treatment deductions. Budget for embryo storage and future FET costs long-term.

Reciprocal IVF vs. Other Options: Cost-Benefit Analysis
Comparing Fertility Treatment Costs for Lesbian Couples
Fertility treatment costs can vary widely depending on the method chosen:
- IUI (intrauterine insemination): $500-$4,000 per cycle + sperm costs.
- Traditional IVF (one partner): $15,000-$25,000 per cycle.
- Reciprocal IVF: $20,000-$35,000+ per reciprocal IVF cycle.
When Reciprocal IVF Is Worth the Investment
- Both partners get a biological connection: one contributes eggs, the other partner carries the pregnancy.
- Strategic role division: use the best egg provider and the best uterine lining to optimize success.
- Shared experience: both partners are engaged in the IVF process.
- Legal protections: in many states, gestational parentage and family-building law is clearer for the carrying partner.
- Success rates can be higher if you optimize egg quality vs. uterine environment.
- Age sweet spot: best when the egg provider is under 35.
- Emotional ROI: for many lesbian couples, shared biological involvement is priceless.
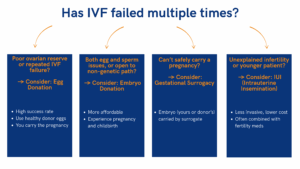
When to Consider Alternatives
- Budget constraints: start with IUI.
- One partner is the clear candidate: if one partner’s fertility markers are strong, standard IVF might be simpler/cheaper.
- Age or medical issues: if the egg provider is over 40 or pregnancy is high-risk, other routes (donor eggs, adoption) may be wiser.
Switching Partners Mid-Treatment
If role reversal becomes necessary (poor ovarian response, embryo quality, uterine issues), you may face another full cycle ($10k-$20k). If you have frozen embryos from Partner A you can transfer to Partner B (cheaper than a second retrieval), but storage and cross-transfer logistics add costs. Plan backups and discuss contingencies with your fertility specialist early.
Your Reciprocal IVF Journey Starts Here
Numbers here are averages. Budget multiple cycles, build a 15-20% contingency, and choose expertise over bargains. If both partners want a biological role, reciprocal IVF often delivers emotional and clinical value that other fertility treatment options don’t.
Ready for real answers? Book a consult with a clinic experienced in reproductive medicine and LGBTQ+ family building.