Mini IVF in Los Angeles – Lower Cost, Lower Stress, Higher Possibility
Starting or expanding your family can feel like an uphill climb, especially if you’ve already faced fertility challenges. At the California Center for Reproductive Health, we understand the emotional and financial weight of that journey, and we’re here to make it gentler.
Understanding Mini IVF & Its Benefits
Mini IVF (minimal stimulation IVF) is a proven, effective option for women and couples who want fewer medications, lower costs, and a more natural path to pregnancy. For many Los Angeles patients, it’s the perfect balance between affordability and advanced reproductive technology.
Unlike conventional IVF, which relies on high doses of injectable fertility drugs, Mini IVF uses oral medications and lower-dose stimulation to encourage the development of a few high-quality eggs.
This means…
Lower Medication Costs
Because Mini IVF requires fewer fertility medications, the overall cost per cycle is often lower. That means less financial stress without sacrificing modern IVF technology.
Reduced Hormone Exposure
For patients worried about side effects, Mini IVF limits hormone exposure. With lower stimulation, you’ll face a lower risk of ovarian hyperstimulation syndrome (OHSS) and fewer uncomfortable symptoms.
More Comfortable, Less Stressful Treatment
Fewer injections, fewer monitoring appointments, and a more natural pace: mini IVF is often described as less overwhelming than traditional IVF.
Comparable Success Rates for Many Patients
While Mini IVF produces fewer eggs, those eggs are often of higher quality. For the right candidates, success rates can be similar to conventional IVF.
Mini IVF versus Traditional IVF
| Cost & Experience Factor | Traditional IVF | Mini IVF |
|---|---|---|
| Medication Use | High doses of injectable medications | Lower doses or oral medications only |
| Monitoring Visits | Frequent (6–8) | Fewer (3–4) |
| Injection Schedule | Daily injections for 10–14 days | Minimal injections, sometimes none |
| Eggs Retrieved | Typically 10–20 eggs | Typically 3–8 eggs |
| Risk of OHSS | Higher risk of ovarian hyperstimulation | Virtually no risk |
| Recovery Time | 3–5 days | 1–2 days |
| Cycle Cancellation | Higher risk of cancellation | Lower risk of cancellation |
| Side Effects | Moderate to severe | Mild to minimal |
| Overall Cost | Significantly higher | Much more affordable |

3,000+

20+

2X
Medication Protocols: Less is More
Traditional IVF relies on the “more is better” philosophy—high doses of hormones to stimulate maximum egg production. Mini IVF takes the opposite approach, using gentle stimulation that works with your natural cycle.
This approach is particularly appealing to women who want to maintain control over their treatment experience and avoid the emotional and physical roller coaster that often comes with high-dose fertility medications.
Success Rates & Realistic Expectations
Traditional IVF might retrieve more eggs, but here’s what matters: live birth rates per quality embryo transferred.
For women under 35, Mini IVF success rates range from 40-50% per cycle, compared to 50-60% for traditional IVF. But here’s the key: Mini IVF costs about 50% less, so you can often afford multiple cycles for the same price as one traditional IVF cycle.
For women over 35 or those with diminished ovarian reserve, the success rates become even more comparable because egg quality matters more than quantity in these cases.
Most successful Mini IVF patients achieve pregnancy within 2-3 cycles. Since the treatment is less stressful and more affordable, patients can often complete multiple cycles in the same timeframe and budget they would have allocated for one traditional IVF cycle.
Are You the Ideal Candidate for Mini IVF?
Women with Diminished Ovarian Reserve
If your ovarian reserve is lower than average, Mini IVF may help you focus on egg quality instead of quantity. Many patients over 38 or those with low AMH levels choose this approach.
Patients Concerned About Ovarian Hyperstimulation Syndrome (OHSS)
With conventional IVF, higher doses of fertility drugs can increase OHSS risk. Mini IVF’s gentle stimulation protocol keeps safety at the forefront, especially for patients with health concerns.
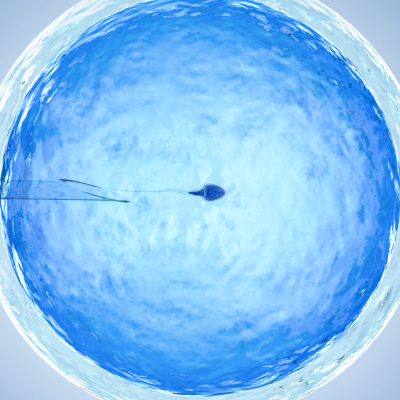
Couples Facing Male Factor Infertility
When paired with intracytoplasmic sperm injection (ICSI), Mini IVF can help overcome male fertility challenges. Even with fewer eggs, high-quality sperm samples can lead to healthy embryos.
Our Mini IVF Process
Initial Consultation & Fertility Testing
Your Mini IVF journey begins with a comprehensive consultation where we review your medical history, previous treatments, and personal preferences. We’ll perform or review recent fertility testing including AMH levels, sperm analysis, and any genetic screening.
Mild Ovarian Stimulation Protocol
You’ll take oral drugs and low-dose fertility treatments to encourage a few eggs to develop.
Your stimulation protocol will be customized but typically includes:
- Days 1-5: Fertility treatments (clomiphene citrate or letrozole)
- Days 6-8: Low-dose injectable hormones (if needed)
- Days 8-12: Monitoring visits to track follicle development
- Day 10-14: Trigger shot to prepare for egg retrieval
Most patients take only one pill daily and require 2-3 small injections total – a dramatic difference from traditional IVF’s daily injection routine.
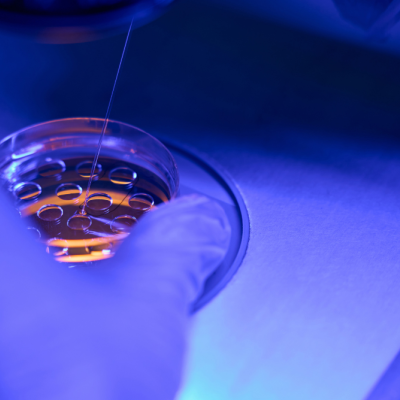
Egg Retrieval
Our egg retrieval procedure is performed in our clinic using the gentlest techniques available. The procedure typically takes 10-15 minutes, and most patients are comfortable enough to go home within an hour.
Embryo Transfer & Pregnancy Testing
After fertilization, the healthiest embryos are selected for transfer.
Embryo transfer is scheduled based on your individual cycle and embryo development. We typically recommend single embryo transfer to maximize safety while maintaining excellent pregnancy rates.
Two weeks after transfer, you’ll return for pregnancy testing.
Mini IVF Cost & Financing Options
Why Mini IVF is More Affordable
Mini IVF is typically more affordable than traditional IVF because it uses lower doses of fertility medications and involves fewer monitoring visits. This streamlined approach reduces costs while still offering excellent outcomes for many patients.
Mini IVF vs. Traditional IVF
Compared to conventional IVF, Mini IVF usually:
-
Requires fewer fertility drugs, lowering medication expenses
-
Involves fewer monitoring appointments and procedures
-
Provides a gentler, simpler treatment plan with a more manageable overall investment
Financing & Payment Options
We understand that affordability is an important part of your fertility journey. To help make treatment more accessible, we offer:
Our team will walk you through all available options during your consultation so you can feel confident moving forward.
Get Started with Mini IVF
You’ve read the facts, heard the stories, and seen the numbers. If Mini IVF sounds like it might be the right fit for your fertility journey, we’re ready to help you take the next step.
Schedule your consultation today and discover why thousands of Los Angeles couples choose us for their Mini IVF.
Don’t wait: your fertility journey deserves a gentler, more affordable approach that actually works!
Success Stories: Real Patients, Real Results
Mini IVF FAQ
What are the benefits of mini IVF?
Mini IVF offers lower medication costs (often 80% less than traditional IVF), reduced hormone exposure, fewer side effects, more convenient scheduling, and virtually no risk of ovarian hyperstimulation syndrome. For many patients, it provides comparable success rates to traditional IVF at a fraction of the cost and stress.
Is mini IVF more successful than traditional IVF?
Success rates depend on your individual situation. For women with diminished ovarian reserve or those over 35, Mini IVF often produces similar or better results per embryo transferred because it focuses on egg quality over quantity. While traditional IVF might have slightly higher success rates per cycle for younger women, Mini IVF’s affordability allows for multiple cycles at the same cost.
Is Mini IVF a good option if I have diminished ovarian reserve (low AMH) or I’m over 38–40?
Absolutely. Mini IVF is often the better choice for women with diminished ovarian reserve because gentle stimulation can produce higher-quality eggs than aggressive protocols. Many women over 38 see excellent results with Mini IVF because the treatment works with their natural cycle rather than against it.
Will Mini IVF reduce my risk of ovarian hyperstimulation syndrome (OHSS) and medication side effects?
Yes, significantly. OHSS risk is virtually eliminated with Mini IVF because we use minimal stimulation. Side effects are also dramatically reduced—most patients report feeling “normal” throughout treatment instead of experiencing the mood swings, bloating, and fatigue common with traditional IVF medications.
How many eggs/embryos can I realistically expect from one Mini IVF cycle?
Mini IVF typically produces 3-8 eggs per cycle, with 60-80% fertilization rates. You can expect 2-5 embryos on average. While this is fewer than traditional IVF, the embryo quality is often higher due to gentler stimulation.
How many Mini IVF cycles will I likely need before I have usable embryos or a pregnancy?
Most successful patients achieve pregnancy within 2-3 Mini IVF cycles. Since each cycle costs significantly less than traditional IVF, multiple cycles are often more affordable than a single conventional IVF attempt.
Will fewer eggs mean fewer chances? Or does Mini IVF produce ‘higher quality’ eggs that offset quantity?
Mini IVF does produce higher-quality eggs that often offset the lower quantity. The gentle stimulation allows eggs to mature more naturally, resulting in better embryo development and implantation rates. Quality is more important than quantity when it comes to successful pregnancy.
How long does mini IVF take?
A Mini IVF cycle takes about 2-3 weeks from stimulation start to embryo transfer. The entire process from consultation to pregnancy test typically takes 6-8 weeks. Treatment is much more convenient than traditional IVF with fewer appointments and less scheduling disruption.
What medications are used in Mini IVF and what side effects should I expect (oral meds like clomiphene/letrozole vs low-dose injectables)?
Mini IVF typically uses oral medications like clomiphene citrate or letrozole, sometimes combined with low-dose injectable hormones. Side effects are minimal—some patients experience mild bloating or breast tenderness, but most report feeling normal throughout treatment.
What is recovery like after egg retrieval in a Mini IVF cycle (pain, downtime, and clinic visit frequency)?
Can you pick gender with mini IVF?
Gender selection through PGT-A genetic testing is available with Mini IVF, though it adds to the cost. However, with fewer embryos produced, gender selection may be less practical than with traditional IVF.
Can we use ICSI or PGT-A with Mini IVF, and does that change success chances or cost?
Yes, both ICSI and PGT-A can be combined with Mini IVF. ICSI is often recommended when there are male factor concerns and may improve fertilization rates. PGT-A can help identify the healthiest embryos and may improve the chances of a successful pregnancy. Both procedures involve additional costs, which our team will review with you during your consultation.
How does the cost of Mini IVF compare to conventional IVF once meds and add-ons are included?
Mini IVF is generally much more affordable than traditional IVF. Because it uses lower doses of medication and fewer add-ons, the overall cost is typically lower while still providing strong outcomes for the right candidates. Even when additional services like ICSI or PGT-A are factored in, Mini IVF often represents a more cost-effective option compared to conventional IVF.