Best Male Fertility Clinics in Los Angeles: 2026 Expert Comparison Guide

Male factor infertility drives nearly half of all conception challenges, yet most fertility centers treat it as an afterthought. A semen analysis isn’t a treatment plan.
This guide evaluates Los Angeles’s top options for male infertility treatments based on specialized expertise, proven microsurgical procedures, success rates, and personalized care.
Whether you’re considering vasectomy reversal, investigating structural issues, or searching for answers after failed treatments, you’ll find the clarity needed to move forward.
| Clinic | Specialty Focus | Best For | Location |
|---|---|---|---|
| California Center for Reproductive Health | General fertility & IVF | Couples needing coordinated specialized male and female fertility care | Encino, West Hollywood, Valencia |
| The Men's Clinic at UCLA | Academic research | Access to cutting edge treatments and clinical trials | Westwood |
| The Turek Clinic | Microsurgical sperm retrieval | Complex testicular sperm extraction cases | Beverly Hills/LA |
| Dr. Mark Zeitlin | Holistic approach | Lifestyle optimization with medical treatment | Los Angeles |
| West Coast Fertility Centers | Multi-location convenience | Couples needing full-service care at multiple sites | Multiple locations |
| Cedars-Sinai Medical Center | Hospital-based care | Complex cases requiring multiple specialists | West Hollywood |
| PFCLA | Collaborative couple care | Unified treatment for both partners | Multiple locations |
| Keck Medicine of USC | Academic protocols | Research-driven treatment approaches | East LA |
California Center for Reproductive Health: LA’s Most Comprehensive Fertility Center
The CCRH advantage: Board-certified reproductive endocrinologists with extensive male fertility expertise, state-of-the-art facilities across three convenient Southern California locations, and personalized care that treats both partners’ fertility factors simultaneously. When you need coordinated care that addresses male fertility within a comprehensive reproductive medicine program, CCRH’s proven success rates and integrated approach deliver results.
Experience comprehensive male fertility treatment:
- Complete diagnostic evaluation: Advanced semen analysis, sperm DNA fragmentation assay testing (SDFA), hormonal testing, genetic screening.
- Medical and surgical interventions: Varicocele repair, hormonal therapies, lifestyle optimization.
- Integrated with IVF/ICSI: Seamless coordination when male factor infertility requires assisted reproduction.
- Sperm retrieval procedures: TESE and other advanced techniques for severe male factor cases.

First consultation: Comprehensive evaluation for both partners with same-day testing capabilities. Clear treatment planning that accounts for male factors, female factors, and optimal pathways to successful conception, through natural conception, IUI, or IVF.
If you want Los Angeles’s highest-ranked fertility clinic with proven male fertility treatment integrated into a comprehensive reproductive medicine program, CCRH combines expertise, technology, and results that other clinics struggle to match.
The Men’s Clinic at UCLA
UCLA brings world class leadership in men’s health research to male fertility treatment. This is where cutting edge treatments get developed before reaching other clinics.
Best for: Complex cases needing multiple specialists, access to clinical trials, or strong IVF integration when male factor infertility requires assisted reproduction.
Trade-offs: Teaching hospital environment means residents during visits, limited appointment availability, and less personalized care than private practices. Plan for lengthy first visits (half-day commitment). Success rates are competitive but outcomes depend heavily on both partners’ factors.
The Turek Clinic
Dr. Paul Turek specializes in getting sperm when others say it’s impossible. If you need microsurgical testicular sperm extraction (TESE) for severe male infertility, this clinic’s pioneered techniques are now used worldwide.
Best for: Azoospermia (no sperm in ejaculate) and complex sperm retrieval cases. Their microsurgical procedures can find viable sperm even in difficult scenarios, enabling biological fatherhood through IVF. Strong fertility preservation for men facing medical treatments.
Trade-offs: Premium pricing for niche expertise you may not need if your case is straightforward (varicocele, reversible obstruction). Educational approach is thorough but can slow treatment timelines.
Dr. Scott Zeitlin
Dr. Zeitlin takes a holistic approach—balancing lifestyle optimization with medical treatment rather than defaulting to surgery.
Best for: Men with borderline semen analysis results who may improve through overall health changes (nutrition, exercise, stress management). Thorough diagnostic work including DNA fragmentation testing.
Trade-offs: Lifestyle-first philosophy can delay surgical treatment when you need vasectomy reversal or varicocele repair. Doesn’t offer advanced microsurgical procedures in-house, and requires referrals for complex cases.
West Coast Fertility Centers
Multiple Los Angeles locations (Santa Monica, Pasadena, Orange County) where both partners receive treatment under one roof.
Best for: Couples needing coordinated care and convenience. Strong in vitro fertilization integration means seamless transitions if male factor infertility requires assisted reproduction. IVF success rates are solid.
Trade-offs: Male fertility can feel like a department within an IVF-focused business rather than the priority. Personalized care varies by location and physician. Male-side diagnostics sometimes move slower than female workup.
Reproductive Fertility Center (RFC)
Takes a broad view of male reproductive wellness, connecting overall health to fertility outcomes.
Best for: Men with erectile dysfunction alongside fertility concerns, or those needing comprehensive evaluation of cardiovascular health, metabolic factors, and hormonal balance. Thorough semen analysis with advanced parameters.
Trade-offs: Doesn’t offer advanced microsurgical procedures: patients needing microsurgical vasectomy reversal, complex sperm extraction, or reconstructive surgery get referred elsewhere. Best for mild to moderate cases, not cutting edge surgical intervention.
Cedars-Sinai Medical Center
Hospital-based program with multidisciplinary expertise for medically complex cases.
Best for: Cancer survivors, men with serious health conditions affecting fertility, or cases requiring urologic oncology expertise. Access to specialists across every medical discipline and full range of reproductive medicine treatments.
Trade-offs: Bureaucratic experience with long wait times, multiple departments, and provider handoffs. Higher costs than private practices. Overkill for straightforward male fertility cases that don’t need institutional firepower.
PFCLA (Pacific Fertility Center Los Angeles)
Treats couples as a unit with simultaneous attention to both male and female factors.
Best for: Couples where both partners have fertility challenges. Coordinated care from semen analysis through IVF. Competitive success rates for male infertility cases.
Trade-offs: Men needing highly specialized microsurgical procedures often need external referrals. System primarily optimized for female fertility: some male patients report feeling like the “junior partner.”
Keck Medicine of USC
Academic medical center combining research expertise with comprehensive urology department.
Best for: Research-driven treatment protocols, complex cases with underlying conditions (hormonal disorders, genetic factors), access to specialists across men’s health.
Trade-offs: Teaching hospital environment with trainees involved in care. Harder to schedule, slower from consultation to treatment. Less personalized than private practices. Protocol-focused rather than agile decision-making.

How to Choose the Right Male Fertility Clinic for Your Needs
Assess Your Specific Fertility Challenge
Different clinics excel at different problems. Match your situation to the right expertise.
- Structural issues (vas deferens obstructions, varicoceles).
Need microsurgical capabilities: California Center for Reproductive Health or Turek Clinic are your best options. Lifestyle changes won’t fix these. - Sperm quality issues without obvious structural causes.
Clinics emphasizing diagnostics (California Center for Reproductive Health, Dr. Zeitlin, RFC) identify underlying causes like hormonal imbalances or infections. - Vasectomy reversal.
Need specialists with proven microsurgical vasectomy reversal success rates. Poor technique can’t be fixed. - Fertility preservation (oncofertility before cancer treatment, surgeries).
Time is critical. Need established protocols and extraction expertise. - Erectile dysfunction affecting conception.
Need integrated sexual health and fertility care.
The underlying cause matters. Don’t pay for microsurgical testicular sperm extraction expertise if medication or lifestyle changes will work.
Evaluate Treatment Philosophy: Holistic vs. Intervention-First
- Conservative, lifestyle-first (Dr. Zeitlin, RFC).
Optimize health before intervention. Avoid invasive procedures, but if your partner is 36, six months on lifestyle optimization costs precious time. - Intervention-focused (California Center for Reproductive Health, UCLA).
Move quickly from diagnosis to treatment. Get faster resolution, but be ready to potentially jump past simpler, most cost-effective solutions.
Personalized care should adapt to you, not funnel you into the clinic’s preferred protocol.
Consider Coordination with Female Partner’s Care
Male fertility doesn’t exist in a vacuum. Coordination with your partner’s care matters, especially when time is a factor.
- Integrated programs (California Center for Reproductive Health, West Coast Fertility Centers): Both partners are in the same system. Smoother scheduling, communication, and coordinated timing for intrauterine insemination or in vitro fertilization.
- Separate specialists: Each partner gets the absolute best expert for their specific issue. If you need complex microsurgical procedures, California Center for Reproductive Health provides deeper expertise than generalist urologists at IVF clinics.
Making separate care work: Your specialists must actively communicate, not just “we’ll send records.” Worst scenario: specialists who don’t communicate, leaving you to translate medical information and coordinate timing yourself.
Geographic and Practical Considerations
- Location and traffic: A Beverly Hills clinic might mean 90 minutes each way from Pasadena. Multiple appointments add up.
- Visit frequency: Initial consultations run 60-90 minutes. Procedures require time off. Some conditions need monthly monitoring; others just a few check-ins.
- Wait times: Top specialists book 4-8 weeks out. If you’re starting chemo soon or your partner is in an IVF cycle, that’s unacceptable. Ask about urgent case accommodations.
- Insurance and costs: Coverage varies wildly. Hospital programs (Cedars-Sinai, UCLA, USC) have better insurance contracts but higher baseline costs. Private practices offer pricing flexibility, but less insurance leverage.
In any case, don’t the prioritize cheapest option: failed cheap treatment wastes more than expensive treatment that works. Understand total anticipated costs, not just procedure pricing. That $3,000 vasectomy reversal becomes $8,000 with facility fees, anesthesia, and follow-ups.

Common Male Fertility Treatments Available in Los Angeles
Non-Invasive Treatments
- Recommended when:
- Borderline semen analysis.
- No structural issues.
- You have time to optimize naturally.
- Lifestyle optimization (assuming you’re not facing urgent timelines):
- Sleep 7-8 hours consistently.
- Improve nutrition (antioxidants, zinc, folate).
- Moderate alcohol consumption.
- Manage stress.
- Exercise (but not excessively).
- Timeline: Sperm takes 74 days to mature, so you need 3-4 months minimum for results. Don’t have time? Skip to medical treatment.
- Medical treatment targets specific problems:
- Low testosterone gets hormone therapy (but testosterone replacement crushes sperm production).
- Infections get antibiotics.
- Hormonal imbalances get medications like clomiphene.
- Success: Repeat semen analysis showing improved count, motility, morphology. If parameters improve but no pregnancy after 6 months, escalate treatment.
Surgical Interventions
- Recommended when:
- Structural blockages.
- Varicoceles causing sperm issues.
- Previous vasectomy.
- Reproductive tract abnormalities.
- Vasectomy reversal reconnects the vas deferens.
- Success depends on years since vasectomy (better if under 10), surgeon skill, and blockages/antibodies.
- Microsurgical vasectomy reversal dramatically improves outcomes.
- Timeline:
- Outpatient (2-4 hours), sperm returns in 3-6 months.
- Pregnancy rates 30-70%, with best surgeons hitting higher end.
- California Center for Reproductive Health is the Southern California go-to, with proven microsurgical expertise and success rates. Turek Clinic also performs reversals, but focuses on cases where retrieval might be necessary.
- Varicocele repair fixes enlarged veins overheating sperm production.
- Only needed when semen analysis is poor and varicocele is significant.
- Microsurgical repair minimizes complications.
- Recovery:
- Desk work in a week, physical activity in 2-3 weeks.
- Sperm improves over 3-6 months.
- Structural corrections address blockages in vas deferens, epididymis, or ejaculatory ducts. But it’s technically demanding, and requires specialists who do these regularly, not occasional general urologists.
Advanced Reproductive Techniques
- Recommended when:
- Severe male factor infertility.
- No sperm in ejaculate.
- Failed surgeries.
- Urgent IVF timelines.
- Microsurgical testicular sperm extraction (TESE) retrieves sperm directly from testicles. Requires significant microsurgery expertise.
- How it works:
- Retrieved sperm used immediately in IVF with ICSI: embryologists inject individual sperm into eggs.
- Don’t need millions of sperm, just a few viable ones.
- Coordination:
- TESE timing must align with partner’s egg retrieval.
- Integrated programs like California Center for Reproductive Health handle it internally, but standalone specialists need careful sync with IVF centers.
- Success:
- Finding viable sperm is TESE success.
- Pregnancy depends on sperm quality, egg quality, and IVF factors; typically 30-50% per cycle.
- Simpler sperm retrieval (PESA, TESA) works when blockages exist, but production is normal. Less invasive, often performed under local anesthesia.
- Fertility preservation (sperm banking) is critical before cancer treatment or fertility-damaging medications.
- Straightforward if there’s sperm in ejaculate.
- If not, it requires surgical retrieval before treatment.
- Urgent cases: Cancer patients can’t wait 8 weeks. California Center for Reproductive Health, Cedars-Sinai, or USC accommodate within days.
- Long-term: Frozen sperm is viable for decades, and can be used for IVF/ICSI, intrauterine insemination, or natural conception.
- Cost reality:
- Retrieval procedures typically cost $5,000-$15,000, plus IVF $15,000-$25,000 per cycle.
- Insurance coverage is inconsistent.
- Weigh surgical correction first (cheaper, time-consuming) versus direct retrieval with IVF (faster, expensive).
What to Expect at Your First Male Fertility Consultation
Initial Evaluation and Testing
- Comprehensive medical history (typically 30-45 minutes) covers: childhood illnesses (mumps affects fertility), previous surgeries (hernias, testicular issues), medications (steroids, testosterone, certain antibiotics affect sperm), sexual history, lifestyle factors (heat exposure, chemical exposures at work), and timeline (how long trying for your first child, intercourse frequency, previous pregnancies).
If your doctor rushes through in 10 minutes, that’s a red flag. Male infertility is detective work, and details matter. - Physical examination (10-15 minutes) checks: varicoceles, testicle size/consistency, vas deferens presence, hormonal imbalance signs. Should feel thorough, not perfunctory.
- Standard semen analysis requires 2-7 days abstinence, collection at clinic (not home), analysis within an hour. Evaluates volume, concentration, motility, morphology.
- What separates good clinics from mediocre: Same-day results versus “we’ll call in a week.” California Center for Reproductive Health, UCLA, and top facilities provide same-day semen analysis, so you leave with actual data, not more waiting.
- Additional testing based on findings: Hormone bloodwork (testosterone, FSH, LH, prolactin), genetic testing if counts very low, scrotal ultrasound if varicoceles suspected, specialized sperm function tests like DNA fragmentation analysis.
- Not every test happens at first visit, but your doctor should explain which are needed and why. Cookie-cutter protocols ordering the same tests for everyone suggest the clinic isn’t thinking critically about your case.
- When to seek help: Standard advice says 12 months if under 35, six months if over 35. But if you already know about a factor (previous vasectomy, testicular issue, fertility-affecting medications), don’t waste time.
Diagnosis and Treatment Planning
- Determining underlying cause: Good specialists synthesize history, exam, and test results into coherent explanation. “Low sperm count” isn’t a diagnosis: it’s a symptom. The diagnosis is why: varicocele causing overheating, hormonal imbalance, blockage from infection, genetic factor, or lifestyle factors.
- Discussion of factors should feel like conversation, not lecture. Your doctor explains: severity of issues, whether correctable versus needing workaround strategies, how male factors interact with partner’s age/fertility, realistic timelines for different paths.
- If your partner is 37 with diminishing ovarian reserve and you have moderate sperm issues, optimal path differs dramatically from a 28-year-old partner with no issues and you having correctable varicocele.
- Treatment options: Expect tiered approach, including conservative measures (lifestyle, supplements, medical treatment), intermediate interventions (medications, minor procedures), definitive solutions (microsurgical procedures, sperm retrieval with IVF).
Your doctor should explain why they’re recommending starting where they are; not just what, but reasoning.
- Red flags: Pushing immediately to the most expensive intervention without explaining alternatives, vague explanations avoiding specifics, dismissing your concerns about approaches you’re uncomfortable with.
- Realistic expectations: Success rates should be specific to your situation, not general statistics. Good clinics provide data: “For cases like yours, e.g., vasectomy five years ago, partner under 35, we see 60-70% achieving pregnancy within a year.” Vague optimism prevents informed decision-making.
- Your path to parenthood: Leave with clarity on recommended treatment, timeline expectations, what happens if first-line doesn’t work, how/when you’ll know if it’s working, coordination with partner’s care.
- Next steps should be documented, not just “follow up in three months” but specific: start medication X, recheck semen analysis on timeline Y, coordinate with partner’s doctor about Z.
- The consultation should feel like partnership, not transaction. If it feels rushed, dismissive, or confusing, trust that instinct: there are better options in Los Angeles.
Your Path to Fatherhood Starts with the Right Fertility Partner
The clinics that deliver results share three elements: specialized expertise in male factor infertility, proven treatment success, and personalized care.
California Center for Reproductive Health stands out as Los Angeles’s highest-ranked fertility clinic with proven high success rates and comprehensive male fertility treatment integrated into cutting-edge reproductive medicine. Whether you need diagnostic evaluation, medical treatment, surgical intervention, or IVF with ICSI, CCRH’s expert team delivers coordinated care that maximizes your chances of successful conception.
Schedule your first appointment for free today and finally get real answers, really fast!
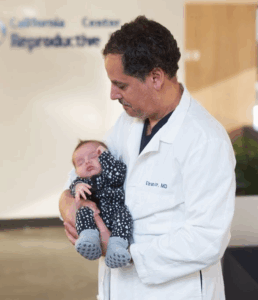
Eliran Mor, MD
Reproductive Endocrinologist located in Encino, Valencia & West Hollywood, CA
Best Male Fertility Clinic in Los Angeles FAQs
How long is the typical wait time to get an appointment at male fertility clinics in Los Angeles?
Top specialists like California Center for Reproductive Health typically book 3-6 weeks out, though they accommodate urgent cases within days. Academic centers like UCLA and USC can take 6-8 weeks due to teaching commitments. If you’re facing time-sensitive issues, ask explicitly about urgent appointment availability: some practices maintain slots that aren’t visible in standard online scheduling.
Does insurance cover male fertility testing and treatment in Los Angeles, or will I have to pay out of pocket?
Most plans cover diagnostics like consultation, semen analysis, and bloodwork as standard medical testing. Hormone therapy and varicocele repair are often covered since they treat medical conditions, but vasectomy reversal is almost never covered because insurers view the original vasectomy as elective. Microsurgical testicular sperm extraction falls in a gray area—some plans cover it, others don’t. Hospital programs like Cedars-Sinai and UCLA typically have better insurance contracts than private practices. Get an itemized cost breakdown before committing to any clinic.
Should I see a male fertility specialist at an academic medical center like UCLA or Cedars-Sinai, or a private clinic?
- Comprehensive fertility clinics like California Center for Reproductive Health: Integrated male and female fertility treatment with strong IVF programs. CCRH leads with highest success rates and advanced male fertility services. Best when coordinated couple care and IVF integration matter.
- Academic (UCLA, Cedars-Sinai): Complex cases, cancer survivors, urologic oncology expertise. Trade-off: residents involved, longer waits, bureaucratic.
Dedicated male specialists (Turek Clinic): Exclusive focus on complex microsurgical procedures like advanced TESE. Best for rare/difficult cases.
How much does a semen analysis cost in Los Angeles, and can I get same-day results?
Basic semen analysis in Los Angeles runs $150-$400 depending on the clinic. Insurance usually covers it as diagnostic testing, though you’ll pay your copay or deductible.
Same-day results should be standard. Top clinics like California Center for Reproductive Health provide results the same day, often within hours.
If I’ve had a vasectomy, should I get a vasectomy reversal or go straight to sperm retrieval with IVF?
Vasectomy reversal makes more sense if it’s been under 10-15 years since your vasectomy, your partner is under 35 with no fertility issues, and you want multiple children. Microsurgical vasectomy reversal costs $5,000-$10,000 with 50-70% pregnancy success rates when conditions are favorable. The trade-off is waiting 3-6 months for sperm to return after the procedure.
Sperm retrieval with IVF is the better choice if it’s been 15+ years since vasectomy (reversal success drops significantly), your partner is over 35 or has fertility challenges requiring IVF anyway, or you need results quickly. The combined cost runs $20,000-$30,000 per cycle, but you get immediate results without the months-long wait.
Some couples pursue a combined approach: attempt reversal first while banking retrieved sperm as backup for IVF if reversal doesn’t work. California Center for Reproductive Health offers coordinated treatment planning to help you choose the optimal path based on your specific situation.
Do both partners need to be treated at the same fertility clinic in Los Angeles, or can we see different specialists?
You can see different specialists: many couples actually do.
- Unified care (California Center for Reproductive Health, PFCLA, West Coast) means seamless coordination and shared records, which prevents timing mishaps for intrauterine insemination or IVF.
- Separate specialists get you the best expert for each partner’s specific issue, but requires active coordination between practices.
Before committing, ask both: “How will you coordinate for IVF timing?” Vague answers typically mean trouble.
What’s the difference between a urologist and a male fertility specialist (andrologist), and which one do I need?
-
- Male fertility specialists: Urology residency + fellowship in male reproductive medicine. Entire practice focused on male infertility. Hundreds of vasectomy reversals yearly.
- General urologists: Handle prostate, kidney stones, erectile dysfunction, cancers. Fertility is small part. Few procedures yearly.
You will need specialists like California Center for Reproductive Health for moderate to severe male factor infertility, microsurgical correction, vasectomy reversal, azoospermia. Success rates are also 30% higher with specialists.
Are there hidden fees at Los Angeles fertility clinics beyond the quoted treatment costs?
Yes. $6,000 vasectomy reversal becomes $9,000-$11,000 with facility fees, anesthesia, post-op, follow-ups. Sperm retrieval + IVF typically cost $20,000+ combined.
If my partner is over 35, does that change which male fertility clinic we should choose in Los Angeles?
Absolutely. Female fertility declines accelerate after 35. Every month matters.
- Prioritize clinics moving efficiently from diagnosis to treatment, same-day testing, no months of conservative approaches first. Don’t optimize your sperm for 4 months while her egg quality declines.
- Consider IVF-integrated clinics that tailor approaches to both partners’ factors,like California Center for Reproductive Health. If vasectomy reversal takes 4-6 months and partner is 38, immediate sperm retrieval with IVF may be better.




