The Benefits of a Mini IVF Treatment
Conventional in-vitro fertilization (IVF) treatments help many infertile couples get pregnant and have a healthy baby. IVF, however, can be time-consuming, invasive, and expensive. If several embryos are transferred to your uterus, IVF sometimes results in pregnancy with multiple babies.
Mini IVF, which is minimal stimulation IVF, is ideal for couples who may be concerned about the high dose of medications used in a conventional IVF cycle, whether you’re worried about the potential physical impact or the financial load.
Here at the California Center for Reproductive Health, our fertility specialists Eliran Mor, MD, and Irene Woo, MD, provide mini IVF as an alternative to conventional IVF to our patients living in the greater Los Angeles area. Read on to learn the benefits of this fertility treatment and see if you and your family could benefit.
The process of mini IVF
Mini IVF simplifies the fertility procedure, resulting in fewer injections, reduced cost, and equal success for appropriate candidates. Mini IVF calls for just a minimal amount of oral medication to stimulate your eggs to produce a small number of high-quality eggs appropriate for fertilization.
During mini IVF, you typically take Clomid or another oral fertility medication daily and have just 1-3 injections of an additional hormonal fertility medication. This is far less than the weeks of injections you might endure with conventional IVF. The entire process of mini IVF takes 7-10 days.
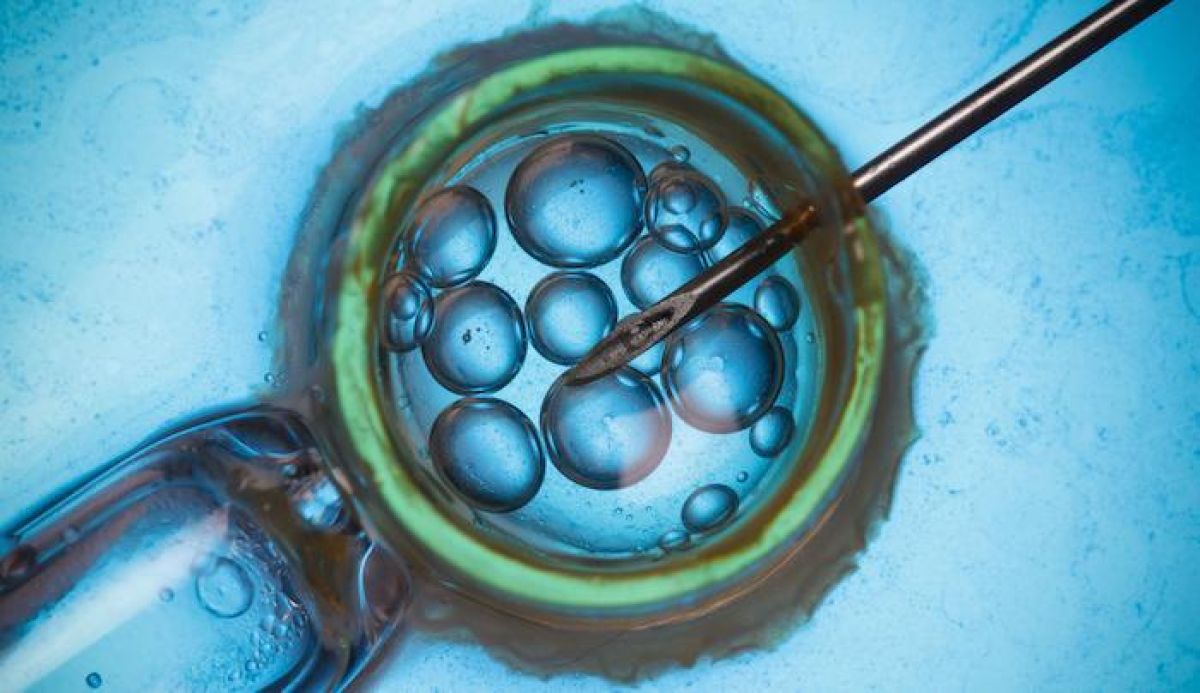
Once the eggs are ready, they’re harvested, viable ones are fertilized in a lab, and the embryos are placed into your uterus in hopes that they attach to the uterine wall to begin a healthy pregnancy.
Mini IVF has many advantages
Mini IVF offers numerous benefits in addition to the hope that you become pregnant. These include:
Lower hormone doses
Mini IVF uses smaller doses of injectable gonadotropins, so the side effects are gentler and easier on your body. Lower hormone dosage means you produce fewer eggs and don’t experience the side effects associated with the excessive levels of estrogen produced by large numbers of eggs.
Lower risk of ovarian hyperstimulation syndrome
Ovarian hyperstimulation syndrome occurs in some women going through the conventional IVF process. The aggressive administration of hormones causes the ovaries to swell and become painful.
Less monitoring
Because mini IVF happens with a lower dose of hormones and medications, less clinical and laboratory monitoring is required. This means you have fewer visits to our office and reduced costs.
Just the right number of eggs
With conventional IVF, the aggressive treatment stimulates the development of many eggs. However, in most cases, just 3-5 of this multitude are actually viable enough for fertilization and implantation. With mini IVF, you usually produce 3-5 high-quality eggs, just the right number for a good chance of developing a healthy embryo. Lower hormone stimulation can produce the highest quality of eggs and improved success rates. This is especially true for older women with poor ovarian reserve.
Fewer fears surrounding multiples
With conventional IVF, the risk of becoming pregnant with multiples is very real. Having more embryos is not necessarily better, as pregnancy with multiples puts you at a higher risk of complications and premature birth.
Candidates for mini IVF
Ultimately, your ability to become pregnant with any fertility treatment depends on your age, the cause of infertility, and your general health. Women younger than 35 with normal ovarian reserves do quite well with mini IVF and often find the procedure more effective than conventional IVF.
Women who are older than 40 may also seriously consider mini IVF if conventional IVF has resulted in poor-quality embryos. Our doctors at the California Center for Reproductive Health review your particular case and can help determine if mini IVF is the right approach for you.
Learn more about the revolutionary effects and methods involved in mini IVF. Call one of our offices in Santa Monica, Alhambra, West Hollywood, Encino, and Valencia, California or book an appointment using the online tool.
Eliran Mor, MD
Reproductive Endocrinologist located in Encino, Valencia & West Hollywood, CA
FAQ
What does a reproductive endocrinologist and infertility specialist do?
Reproductive endocrinology and Infertility is a sub-specialty of Obstetrics and Gynecology. In addition to managing medical and surgical treatment of disorders of the female reproductive tract, reproductive endocrinologist and infertility (REI) specialists undergo additional years of training to provide fertility treatments using assisted reproductive technology (ART) such as in vitro fertilization.
Reproductive endocrinologists receive board certification by the American Board of Obstetrics and Gynecology in both Obstetrics and Gynecology and Reproductive Endocrinology and Infertility.
When should I see an REI specialist?
In general, patients should consider consulting with an REI specialist after one year of trying unsuccessfully to achieve pregnancy. The chance of conceiving every month is around 20%, therefore after a full year of trying approximately 15% of couples will still not have achieved a pregnancy.
However, if a woman is over the age of 35 it would be reasonable to see a fertility specialist earlier, typically after 6 months of trying.
Other candidates to seek earlier treatment are women who have irregular menses, endometriosis, fibroids, polycystic ovary syndrome (PCOS), women who have had 2 or more miscarriages, or problems with the fallopian tubes (prior ectopic pregnancy).
What are the reasons we are having trouble conceiving?
Approximately 1/3 of the time cause for infertility is a female factor, 1/3 of the time a male factor, and the remaining 1/3 a couples’ factor.
At CCRH, we emphasize the importance of establishing a correct diagnosis. Both partners undergo a comprehensive evaluation including a medical history and physical exam.
Furthremore, the woman’s ovarian reserve is assessed with a pelvic ultrasound and a hormonal profile. A hysterosalpingogram (HSG) will confirm fallopian tube patency and the uterine cavity is free of intracavitary lesions. A semen analysis is also obtained to evaluate for concentration, motility, and morphology of the sperm.
Additional work up is then individualized to direct the best possible treatment option for each couple.
What is IVF? What is the process like?
In vitro fertilization (IVF) is the process that involves fertilization of an egg outside of a woman’s body.
The process starts with fertility drugs prescribed to help stimulate egg development. In your natural cycle, your body is only able to grow one dominant egg, but with stimulation medication we can recruit multiple eggs to continue to grow. After about 8-10 days of stimulation, the eggs are surgically retrieved and then fertilized with sperm in a specialized laboratory. Fertilized eggs are then cultured under a strictly controlled environment within specialized incubators in the IVF laboratory for 3-5 days while they develop as embryos. Finally, embryos (or an embryo) are transferred into the uterine cavity for implantation.
Should I have IVF?
Before deciding if IVF is the right choice, it’s important to sit down with an REI specialist to discuss available treatment options. For some people, other methods such as fertility drugs, intrauterine insemination (IUI) may be the best first choice treatment. At CCRH, we believe each individual couple is unique and not everyone needs IVF.
Is the IVF procedure painful?
While not painful, the fertility medications may some side effects including headaches, hot flashes, mood swings, and bloating. The injection sites may also bruise.
Will IVF guarantee a baby?
Unfortunately, no. Many people think once they start IVF it’s a matter of time that they will be pregnant and have a baby. But according to national statistics per the Society of Assisted Reproduction (SART), on average 40% of assisted reproduction cycles achieve live births in women under age 35. The chances of success then continue to decrease with advancing age.
At CCRH, we employ only evidence-based interventions to ensure patient safety and optimal outcome. While we cannot guarantee a baby, we guarantee that you will receive the best, most advanced, personalized care to help you maximize your chance of a baby.
What is the success rate for IVF?
The average IVF success rate (success measured in live birth rate) using one’s own eggs begins to drop around age 35 and then rapidly after age 40. This is due to the decline in egg quantity and egg quality as a woman ages.
Our clinic’s success rate consistently beats the national average year after year.
Do insurance plans cover infertility treatment? How much does IVF cost?
Individual insurance plans often do not have any coverage for infertility treatments. If you have a group plan, you can call members services to see if they have coverage for infertility (including consultation/workup and IVF).
After your consultation with our REI specialist, one of our dedicated account managers with sit with you to go over the cost of treatment.




