Infertility Treatment Options for Women Over 40
Infertility Treatment Options for Women Over 40
If you weren’t really ready to start a family way back when you were in your 20s, you’re not alone. Pursuing a higher education, advancing your career, traveling the world, building a home, and finding the right person to share your life with takes time, and many women today find themselves trying to conceive for the first time when they’re in their late 30s or early 40s.
You may be worried about your chances of conceiving naturally if you’ve heard that being past the age of 35 can simply make it harder to become pregnant, or that being past the age of 40 means you may not be able to conceive without some type of reproductive assistance.
While it’s true that the average 40-year-old woman has far fewer high-quality eggs than she did in her 20s, your personal chances of conceiving depend on a variety of factors, not just the number of candles on your last birthday cake.
Here at California Center for Reproductive Health, we take an urgent and individualized treatment approach for women over 40 who’ve had trouble conceiving naturally. Here are some of our most successful strategies.
Infertility evaluation
It’s impossible to begin an individualized fertility treatment protocol without first undergoing a preliminary infertility evaluation. For women over 40, infertility is generally defined as the inability to become pregnant after six months of regular, unprotected sexual intercourse.
In many cases, a comprehensive infertility evaluation can be completed within one or two menstrual cycles. The evaluation process requires a detailed medical history and physical exam, including a variety of lab tests and imaging tests. Depending on your unique case, you may undergo hormone testing, ovulation testing, or pelvic ultrasounds to pinpoint or rule out certain conditions or structural issues.
Lifestyle changes
When you’re in your 20s, it’s fairly easy to lead a relatively unhealthy lifestyle and still become pregnant. But once you hit your mid-30s and beyond, making consistently healthy lifestyle choices is key to protecting and promoting fertility.
As the quantity and quality of your eggs decline, it’s increasingly important to double down on healthy habits to ensure you’ve done everything you can to support your body’s reproductive system. Eating a nutritious diet, staying moderately active most days of the week, quitting smoking, and avoiding alcohol are several important steps you can take toward optimal fertility.
Another key change you may need to make is achieving a healthy body weight. Being overweight or significantly underweight can make it more difficult to become pregnant because both conditions can impact your estrogen levels and interrupt normal ovulation, which is the monthly release of an egg from one of your ovaries.
Many women in their late 30s and early 40s are surprised to learn that reaching a healthier body weight is sometimes all it takes to reestablish normal ovulation and make pregnancy possible.
In vitro fertilization (IVF)
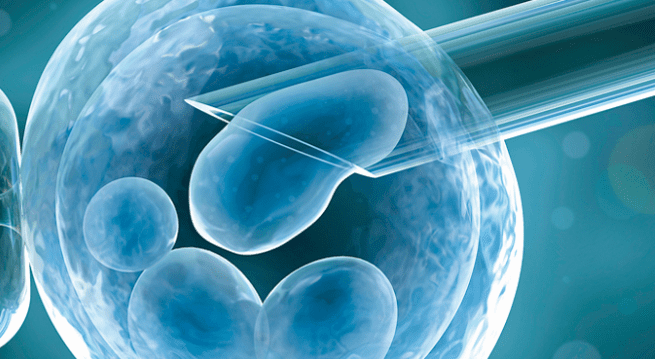
Although healthy lifestyle changes are an important piece of the fertility puzzle, these changes aren’t always enough to complete the picture. In such cases, in vitro fertilization (IVF) with ovarian stimulation is often one of the quickest and most reliable treatment options for women over 40.
During IVF, your ovaries are stimulated with injectable fertility medications so they produce multiple eggs, which are then surgically removed and fertilized in a lab with your partner’s sperm or donor sperm. The fertilized egg grows in a strictly controlled environment for up to five days before it’s transferred to your uterus, where it’s meant to implant itself in your uterine lining and continue to develop.
Although IVF success rates for women using their own eggs begin to decline rapidly starting at about the age of 38, a significant number of women over the age of 40 — and up to about the age of 44 — have experienced IVF success using their own eggs.
At the California Center for Reproductive Health, our IVF success rates for women ages 41-42 is about one-and-a-half times better than the national average. For women over 42, our IVF success rate is about four times better than the national average.
Egg donation considerations
As you get older, it’s important to keep in mind that the age of your uterus is far less important than the age of your eggs, simply because egg quality declines rapidly once you’re over 38. That’s why if you’re over the age of 40 and haven’t had success with IVF using your own eggs, you may want to consider using donor eggs to help make your family dreams a reality.
Although many women view using donated eggs as a sort of last-resort treatment, it’s an ideal option from the standpoint that it offers a much higher success rate than IVF treatments using older eggs.
In fact, IVF done via egg donation results in higher success rates than many other types of assisted reproductive technology, making it a wonderful alternative for women who don’t have success with other treatment methods, including IVF with their own eggs.
If you’re over 40 and you’re ready to make your family dreams a reality, call one of our clinics in Encino, West Hollywood, Monica, or Valencia, California, or use the convenient online tool to schedule a fertility consultation today.